37 min read • Healthcare & life sciences
A bold vision for India’s digital health
A digital revolution driven by the Indian consumer awaits
FOREWORD
Across the healthcare spectrum, technological innovations continue to be developed and made available to consumers at breakneck speed. Within this evolving healthcare landscape, care is becoming more personal, more patient centric, less episodic, more omnipresent, and fully embedded in the lifestyles of the population. Innovative use of digital technologies therefore creates opportunities to enhance patient experience and at the same time optimize care delivery to ensure affordable health access to all. Resulting changes in the fundamentals of healthcare delivery affect all components of the healthcare value chain — from outpatient care enabled through telemedicine, to inpatient care optimized through remote care and home health enabled through digitalization, Internet of Things (IoT), and other interventions.
The COVID-19 pandemic has catalyzed both technological and behavioral change — on one hand, forcing people to embrace digital innovations in all areas of life and especially healthcare, and on the other, creating significant pressure on health systems and exposing supply chain lacunae globally. As a large and growing healthcare market and a hub for innovation and digital entrepreneurship globally, India is poised to see a paradigm shift in digitally enabled healthcare. In this context, this Report seeks to explore how global trends and success stories in digital health will be relevant in the Indian context, what opportunities could emerge in the near future, how ready the ecosystem is to adapt to the changing landscape, how recent policy interventions have set the stage for accelerated adoption of digital health, as well as what specific challenges may need to be overcome and how these translate into innovation opportunities for Indian healthcare players.
- Barnik Chitran Maitra, Managing Partner, ADL India & South Asia
- Shravan Subramanyam, President, NATHEALTH, CEO, GE Healthcare
- Siddhartha Bhattacharya, Secretary General, NATHEALTH
- Vikas Kharbanda, Partner, Healthcare & Life Sciences, ADL Middle East
EXECUTIVE SUMMARY
Digital technology has a transformative power that eclipses the capacity of any other force behind earlier socioeconomic revolutions. In healthcare, digital technology is creating a quantum shift, one that could transform healthcare in India almost beyond imagination. India could have 1 billion digital health users by 2030, enjoying an inclusive health system where healthcare keeps expanding but costs keep falling — a system that efficiently prevents and treats diseases and responds to individual lifestyles and disease profiles with tailored treatments, all at an affordable price.
This is a future that the digitization of healthcare can achieve. But only if the stakeholders involved step up to the challenge.
The demand already exists. India already has 400 million digital health users, using available services such as telehealth, home health, home testing, e-pharmacies, and other digitally powered offerings, even without much innovation by large healthcare providers. A survey by Arthur D. Little (ADL) to identify what drives digitized healthcare adoption in India showed up to 65% acceptance of digital health solutions among customers who use e-commerce services. Significantly higher adoption of digital health tools was reported by patients who had long-term disorders such as cardiovascular disease, diabetes, and hypertension. The pandemic forced people to use digital channels for care needs. Having experienced the benefits of digitally enabled healthcare delivery, consumers now consider them a necessity.
However, as too often in India, supply lags well behind demand. The underpinnings are already there — India now has a sturdy digital backbone via Ayushman Bharat Digital Mission (ABDM). Aiming to capture health data across physicians, providers, and patients, the platform promises interoperability, flexibility, security, scalability, and wide access.
It is now up to healthcare providers, start-ups, technology providers, investors, and other stakeholders to develop digital health offerings that meet and stimulate demand. Like nature, the economy abhors a vacuum — those who tarry could find that others have already captured the opportunities.
At the moment, opportunities abound. What India needs is effective, accessible, and high-quality healthcare solutions that provide equitable access and that can be rapidly deployed and scaled up. Conventional healthcare capacity is highly unlikely to catch up with the demand and supply gaps the country suffers now. Digital solutions are the answer, building on the deep penetration of smart devices and increases in connectivity that the country has invested in over the past decades.
The pandemic catalyzed the adoption of telehealth, home health, home testing, e-pharmacies, and other digital offerings. But there is still a lot of room for growth. Meanwhile, some solutions remain largely unexplored, including e-diagnosis and tech-enabled home health and more mature e-pharmacy solutions.
For conventional healthcare players, health technology start-ups, and investors, this is the time to enter and build a hard-to-beat position. How they could do so and the policy and regulatory support they will need can be summarized as follows across 11 imperatives:
Provider imperatives
- Develop “digital first” strategies instead of “digital as a bolt-on” for conventional businesses.
- Create digital health offerings that are integrated — from preventative health to patient first contact to point-of-care delivery, onward to post-care follow-up and then recuperative care.
- Orchestrate partnerships and build-buy partner strategy.
- Set a clear data strategy to use data to improve the health system.
Payer imperatives
- Develop digital distribution strategies focusing on customer ease and accessibility.
- Build health claims platforms to improve efficiency and reduce risks and fraud.
Regulatory imperatives
- Develop regulatory framework for policy that pushes legacy players toward adopting digital health offerings while providing trust in digital solutions, data security, and consumer satisfaction.
- Encourage start-ups through the right regulatory and policy support.
Investor & funding imperatives
- Develop an attractive, independent investment ecosystem for digital-first healthcare plays as opposed to digital health investments — with digital as a key parameter for investment ideation, deal identification, transaction screening, and post-deal value creation.
- Start targeting brick-and-mortar services from an integration perspective where some momentum is already observed (notably with large players like Practo and Pristyn Care).
- Finance digital health innovations and platforms through greater emphasis on healthtech and insurtech start-up ecosystems.
1
GLOBAL HEALTH TECH ADOPTION TRENDS & DELIVERY INNOVATIONS
Key trends impacting healthcare sector
The future of healthcare is being shaped by several trends. Fundamental shifts in demand and epidemiological characteristics, demographic and access improvement in healthcare, emphasis on supply chain resilience, changing consumer preferences and views on healthcare, increasing automation, standardization, and efficiency are driving the evolution of the healthcare sector as well as digital health and health tech innovation.
Globally, noncommunicable diseases (NCDs) are expected to drive a lion’s share of disease burdens, according to the World Health Organization.[1] NCDs are already the leading cause of mortality and disease burdens globally, contributing to over 70% of deaths globally before the COVID-19 pandemic. The shift has already permeated from developed countries to developing countries and notably India as well. As many as 77% of NCD deaths globally now occur in developing countries like India. Key ailments like cardiovascular diseases, cancers, respiratory diseases, and metabolic disorders drive a majority of the mortality burden in India as well.
Notwithstanding the impact of COVID-19 in the short term, comorbidities and risk factors such as diabetes, hypertension, and cardiovascular susceptibility are well known to have driven significantly higher mortality among vulnerable patient groups during the pandemic as well.
As life expectancy increases globally, and especially so in developing markets, the need for healthcare services is expected to increase significantly as well. In fact, the expected increase in the proportion of people above the age of 60 is set to grow 1.5 times over the next 20 years (14% in 2021 to 20% in 2040).[2] Access to better healthcare must improve at the same time to enable a healthy population to thrive and grow.
During this period, the elderly population (those people older than 80 years old) is likely to grow from about 125 million globally to over 434 million by 2050, with sizable growth in this demographic being contributed to by large and (currently) developing markets like India. Public health agencies and experts also suggest that the incidence of long-term ailments and chronic conditions such as dementia and Alzheimer’s will continue to grow. Estimates point to an increase of this incidence from 47 million in 2015 to 75 million by 2030.
Demand for this demographic segment currently has larger scale in developed countries with older demographic bases. However, as the populations in developing countries age further, the younger population ages, and fertility rates stabilize, developing economies can also expect to see the elderly segment becoming increasingly critical.
Healthcare delivery paradigm shift
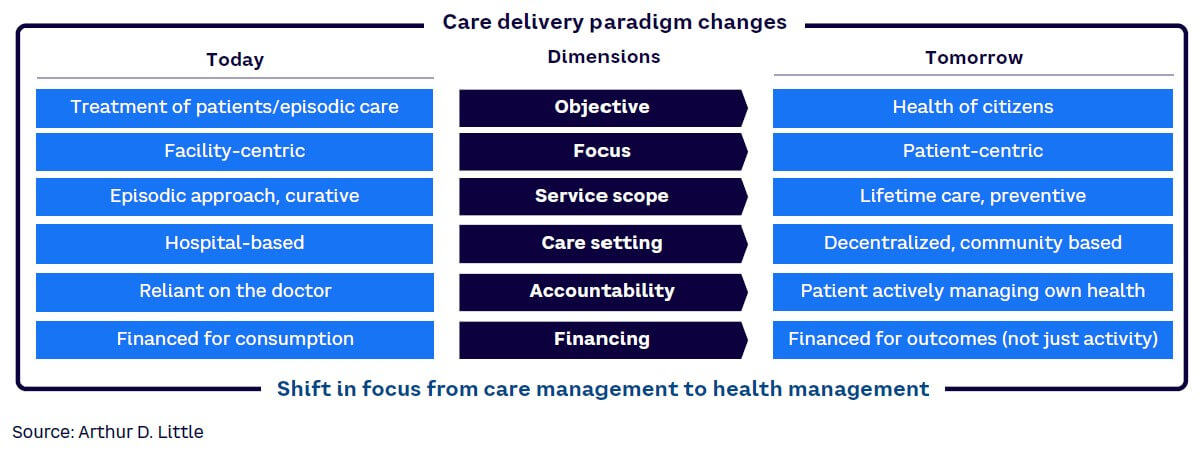
As the need profile evolves, the care delivery approach to address the demand is also evolving. All dimensions of the care delivery paradigm are being impacted — from overall targeted objectives and design criteria for the healthcare ecosystem, to focus of treatment, service delivery approaches, novel care delivery settings for optimization, shifting accountabilities of health outcomes from physicians to a collaborative approach with patients, to funding of health systems on activity basis to an outcomes/outputs basis (see Figure 1).
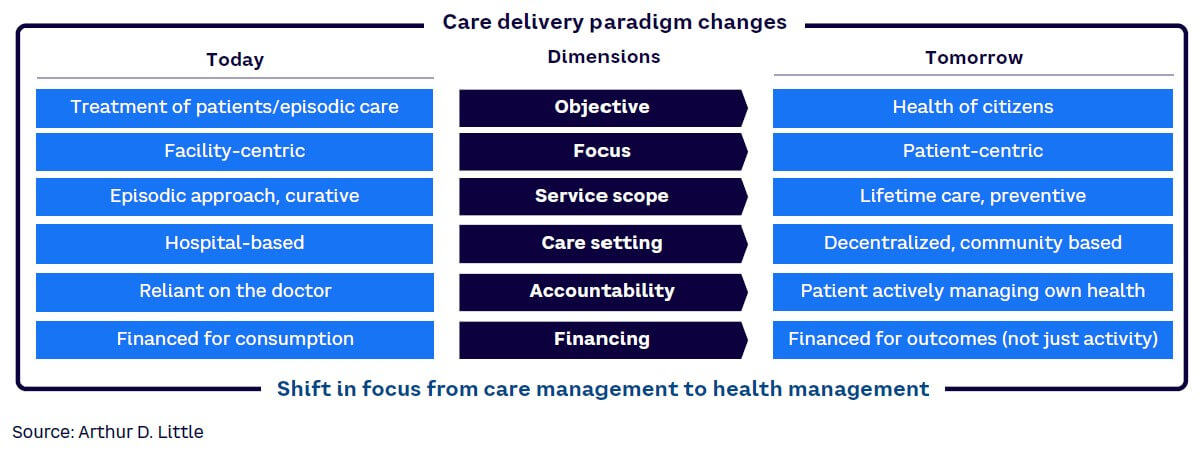
The emerging paradigm will force care delivery models to go beyond just delivering care outside the provider infrastructure and start to make healthcare more omnipresent with the health consumer. Specifically in an Indian context, care delivery models need to also evolve and create more equitable and democratic access — servicing the marginalized and at-risk population groups more effectively. Tech-enabled business models in healthcare therefore likely need to be rethought to create infrastructure and service offerings designed for such delivery modalities.
2
GLOBAL TRENDS IN DIGITAL HEALTH & ENABLEMENT
Technology-enabled change in the healthcare space has also seen significant acceleration in recent years, especially from the perspective of development of new treatment modalities and changes in clinical methods. Even traditional areas of technological adoption have seen significant and rapid growth. New vaccine developments are a benchmark example of effective technological adoption in fundamental healthcare delivery. Complex vaccine development activities, typically taking years or decades, have been accelerated to be completed in months due in large part to technological advances in genomic sequencing, collaborative research with leading universities and research programs, and rapid scale-up of technological offerings.
Shift from information digitalization to digital health
Use cases of digital technologies in healthcare target a shift in the way information is received and processed in the healthcare system. The emphasis of emerging, scale-based solutions is to move away from pure digitalization of information toward developing digital solutions in care delivery.
Health data, at the same time, is diverse and collected across a variety of platforms in a complex healthcare ecosystem. Systemic sources of information could be supplemented by data and interpretation of physical testing/diagnosis.
The diversity and lack of unified structure in collected information represents challenges that can be addressed at scale. Connecting collected data from patients and filtering relevant information for clinical decision making is critical for efficient and effective care delivery. Additionally, the availability of standardized, curated, and accurate information regarding patient demographics, health history, prior complications, comorbidity status, and severity are all critical decision points that can be integrated for clinical decision making.
Scale-based clinical data collection and standardization can then support health information networks and exchanges that enable research activities such as clinical trials, payor optimization, and transfer of information among different health information systems that may be in large-scale use, in addition to supporting treatment decisions by physicians.
Remote health & virtual care delivery becoming mainstream
With patient care moving away from facility-based treatments to virtual models, ecosystems trending toward maximizing care access to all patient groups, and improving access to telecommunications infrastructure, multiple remote health and virtual care use cases are gaining significant traction globally. These include offerings across the entire spectrum of patient care — from telediagnosis and teleconsultation services, which are lower complexity in overall delivery, to electronic ICUs (e-ICUs) and virtual hospital concepts.
The e-ICU platform is a centralized model in which nurses, doctors, and administrators are connected to one or more satellite ICUs. The platform combines audio/visual technology, predictive analysis, data visualization, and advanced reporting to overcome ICU capacity constraints and extends critical care to patients regardless of their location. Advanced clinical decision support analytics enable providers to intervene at the earliest indication of patient deterioration.
Telemedicine, virtual hospitals, and e-ICU concepts have already seen mainstream traction, catalyzed by COVID-19-related travel restrictions and infection issues. In addition, the use cases for telemedicine concepts also allow for lower-cost/higher-volume countries like India to become referral centers for higher-income, lower-volume countries.
COVID-19: Catalyst of change in digital health
COVID-19 has had a significant impact on the growth of technology and digital solutions across several use cases in healthcare globally. Solutions, including digital tools such as teleconsultations, virtual diagnosis, digitalized mental health support, home testing and report generation, and e-pharmacies have, as a result of the COVID pandemic, become more personalized, cognitive, and integrated within the lives of patients and providers. ADL’s interviews with senior leaders indicate that a large number of the beneficiaries/early adopters of these programs have been patients with chronic ailments with a need for periodic follow-ups and patients who require significant post-acute recuperative care as well as those in vulnerable comorbidity groups.
Potentially scalable consumer use cases
AI/ML-enhanced decision making and automation
A broad set of offerings powered by artificial intelligence (AI)/machine learning (ML) applications in healthcare are gaining traction globally. First, tools that support clinical decision making, diagnostics, laboratory, and other direct care delivery aspects are becoming increasingly automated and diagnostics/lab reviews, decision-making support short of consultations, and other care delivery automation activities are under consideration. Second, AI/ML applications in nontherapeutic interventions in mental health and wellness are also undergoing exploration. Third, AI/ML solutions that automate and enhance routine processes such as coding, logging, case tracking, and documentation activities post procedure are also targeting efficiency- and physician-bandwidth-enhancement opportunities. Natural language processing (NLP) applications through chatbots also enable patient information capture, supporting preliminary self-diagnoses for pre-consultation reporting and pre-diagnosis/lab prep, and can enhance efficiency.
Health personalization
With a shift away from episodic care toward preventative care, personalization of health is becoming a key focus area within the digital health space. Consumers of health services are also more aware than ever before that personalization options for healthcare needs exist in the market. Personalized health solutions can therefore be a critical component of the overall preventative care approach in the market, and gamification and rewards can further be used to help ensure that digital healthcare is embedded in the lifestyles of patients.
Several technological developments, such as miniaturization and acceptance of wearable devices by the population, support adoption of personalized healthcare. As technological maturity remains lower than the levels required to enable clinical interventions through wearable tech, the segment is currently restricted to higher-level health data metrics, as other health sensor technologies become mainstream. Consensus estimates of growth in the wearables segment point to 13%-15% growth over the next five years, with the market volumes set to grow three-fold over the next four to five years, to close to 775 billion devices every year.[3]
AR/VR for training and care delivery
With COVID-19 creating significant travel barriers since 2020 and increasing prevalence of low-latency, high-speed network connectivity worldwide, augmented reality (AR)/virtual reality (VR)-based applications are gaining significant traction. AR/VR-based healthcare training for physicians, specialized technicians, and other clinical delivery staff are becoming increasingly mainstream globally, especially in surgical and other specialized therapy areas where availability of physical trainers may be limited. Mixed reality offerings also can offer not just the audiovisual experience but significant components of tactile feel in several therapy areas. In addition, patient-linked use cases for AR/VR are also likely scalable and appropriate for managing and enhancing functional outcomes in patients with behavioral and developmental disorders.
AI for detecting cardiac conditions
Some clinical conditions such as cardiac arrests and stroke can be effectively prevented with early detection and intervention. AI can be used to analyze data sourced from multiple sources such as wearables, patient checkups, and patient vitals to effectively predict life-threatening events such as cardiac arrests. An AI system has been used in Copenhagen, Denmark, to analyze sounds during emergency calls and alert dispatchers with 92% accuracy.
Home hospitals
Building hospitals entails high CAPEX investments with a long breakeven period. To reduce the CAPEX outflow and provide care nearer to patients, some health systems have experimented with home hospitals. These utilize telemedicine, AI, clinical decision-making software, and remote sensing to connect patients and caregivers. The caregivers are provided with real-time data on the condition of patients and assistance on treatment planning and interventions. Caregivers are also alerted to move patients to a higher care facility if needed. This provides a mix of continuous patient monitoring at a lower cost of delivery of treatment for patients.
Predictive modeling
The COVID-19 crisis illuminated capacity planning and surge flow management challenges at the healthcare system level. As a result, facilities and policy makers now capture large amounts of data — from clinical indications to case progression, geospatial data, and clinical and nonclinical demographic data. Predictive modeling may allow multifactor analysis and identification of growth and evolution patterns in epidemiology to assess capacity requirements on a dynamic basis. For example, electronic medical records are being used to detect patterns and estimate the number of hospital visits, number of patients who would return to the hospital within a given number of hours, length of stay, and so on. Researchers at St. Michael’s Hospital in Toronto, Canada, have developed an algorithm that can predict the number of visitors to the emergency department with 95% accuracy, depending on the day of the week, relationship to major holidays, temperature, and climate.
3
SELECT GLOBAL STUDIES
Digital health offerings are accelerating innovation and are deeply impacting procurement functions in the healthcare sector. Healthcare facilities tend to utilize a wide variety of consumables. In fact, a typical healthcare facility may stock several thousands of medical product types and SKUs within their inventory and include tens to hundreds of thousands of SKUs within their overall formulary for procurement and usage.
These products are also widely varied in their characteristics. For example, storage requirements such as temperature, humidity, lighting, and so on, may vary significantly and have a direct impact on quality of clinical outcomes. Clinical shelf life for products may vary from a few months to a few years. Technological changes to products and delivery mechanisms may change. Product recall and safety management create complexity in supply chain management. Products — from lower-cost, basic medications to high-end, high-valued medical devices to legally controlled substances — need to be procured, stored, managed, and tracked through a unified ecosystem by healthcare enterprises. Critically, from an enterprise-viability perspective, procurement cost and pilferage risks may be high or prohibitive as well, which healthcare organizations need to balance. All these complexities necessitate a responsive, effective, and adaptive supply chain management solution for healthcare players.
Big data and tech-enabled use cases in procurement thereby potentially enable the adoption of value-based procurement opportunities in the healthcare sector.
The Indian market has its unique share of challenges in this context, given the increased need for cost-efficient solutions. Given the lower affordability of healthcare in the country and lower penetration of health insurance among the population base, viability of specific use cases for supply chain management remains a key area to improve accessibility. Leading CTOs/CIOs in India’s healthcare space interviewed by ADL make the case for data-driven and digitally enabled procurement. They also highlight the criticality in six areas:
- Right usage of hard technology for product identification and segregation based on the need for and value of the product versus the investment required to collect information on product stocks/usage.
- Standardization of materials for procurement.
- Effective governance around the supply chain to ensure appropriate usage of materials.
- Genuine integration with financial systems and employing tech platforms at their core.
- Transition planning from nondigital approaches to digital approaches.
- Multidisciplinary team engagement at the solution design phase and training of the workforce to ensure alignment with targeted procurement outcomes.
4
INDIAN DIGITAL HEALTH LANDSCAPE
Key constituents of digital health in India
Most prominent and mature digital health platforms in India have historically targeted enhancement of front-end consumer-facing activities within the care pathways. Penetration of services has largely centered around activities peripheral to core healthcare delivery. Activities such as scheduling of visits and appointments, physician/practitioner identification, home diagnostics/sampling, and case history management have seen traction in the Indian marketplace.
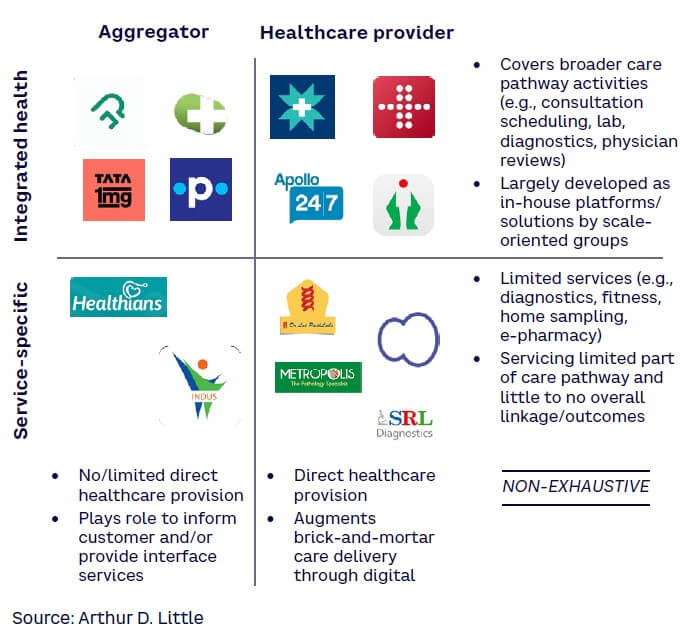
Consumer-facing activities comprise four broad categories of product suites (see Figure 2):
- Integrated health provider applications — covering a wide variety of healthcare activities, including physician selection, appointments, labs and testing, medical records, and other associated core healthcare delivery services. Additional activities in this category that may be provided also include allied services such as claims and payment management, billing, and so on. These applications are developed primarily by large-scale players with significant capacity, geographical outreach, and internal system maturity to support integration of offerings. The targeted value proposition for these applications is to ensure customer “stickiness,” patient relationship management, and long-term convenience for patients — especially for chronic care cases.
- Service-specific health provider applications — including a limited but selective offering of specialized services such as labs, diagnostics, dentistry, and so on, with key services including scheduling, home pickup of samples, and report delivery. The targeted value proposition for these applications is largely to expand outreach and enable wider patient capture on a shorter-term basis.
- Integrated health aggregators — covering a wide variety of services, including consultation scheduling, teleconsultations, lab sampling, diagnostics selection, and so on, but with no/limited support from brick-and-mortar infrastructure under the provider’s own umbrella. The primary focus in this category is to enable differentiation through better information sharing with patients and their family members.
- Service-specific health aggregators — including narrow/niche segments of care delivery, operating as information-sharing platforms with consumers and aggregation within a limited service set.
From an operations standpoint, a variety of digital offerings have been deployed by healthcare providers in the country. These span information management applications such as health information system platforms, supply chain management and vendor management platforms to integrated financial and management reporting systems.
Digital health adoption & acceptance among Indian consumers
To understand the core drivers underpinning the digital health consumer in India, ADL commissioned a broad-based consumer survey administered across the country. Longitudinal data collected from prior surveys and focus group discussions were also used to draw upon and understand recent trends and validate findings. Several key trends have been observed in the customer survey that bring to light the behavioral trends observed among digital health consumers in India:
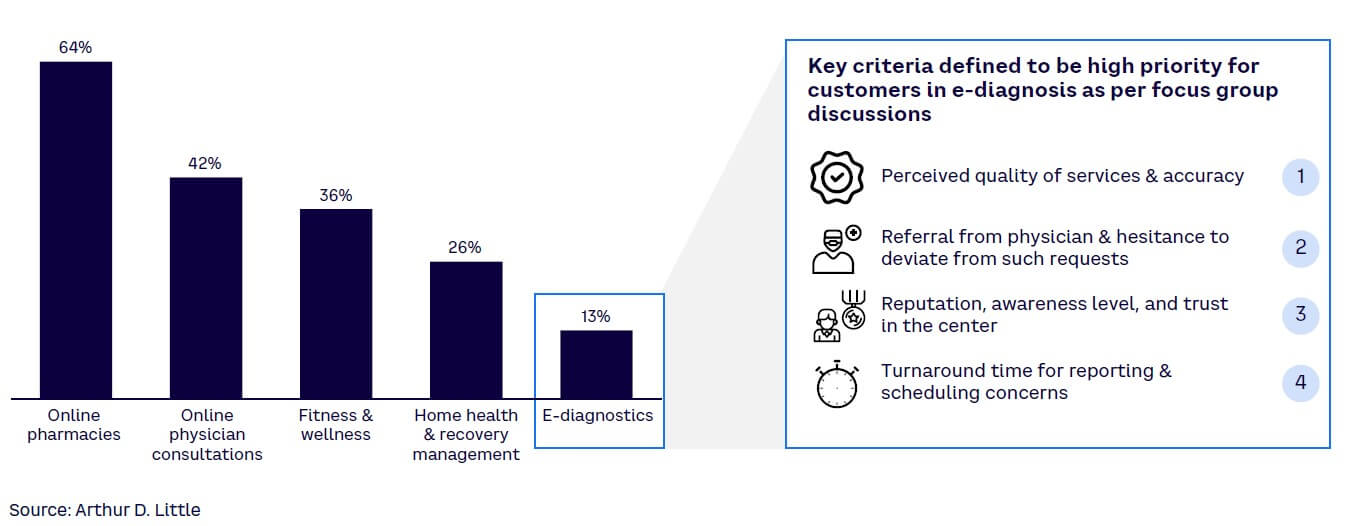
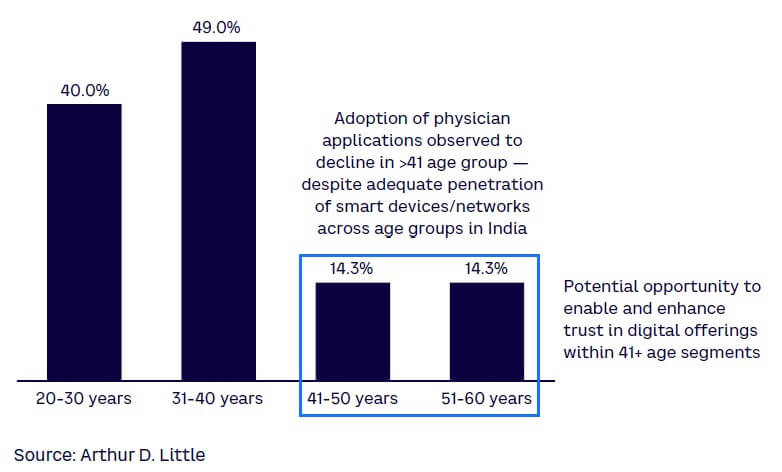
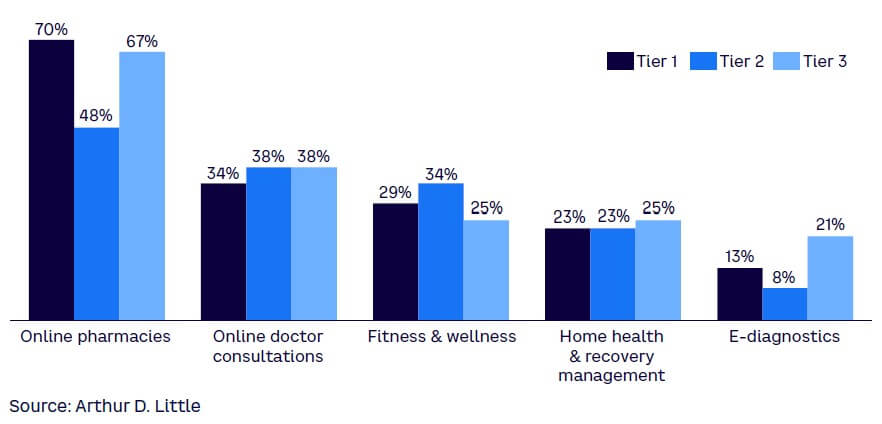
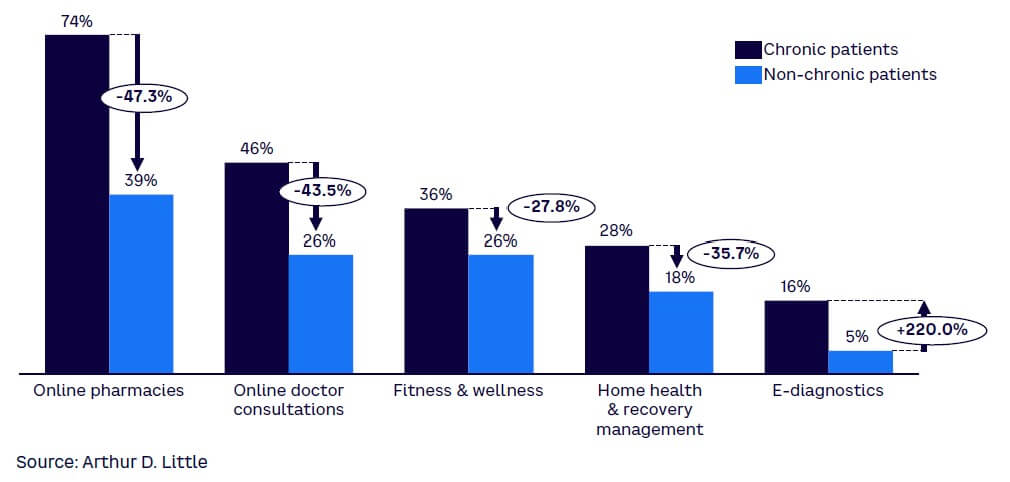
- Deep penetration of digital health solutions, with significant room for growth. ADL’s survey indicates significant traction among consumers on the use of online pharmacies, physician consultations, and fitness and wellness applications (see Figure 3). All these applications observed between 35%-65% acceptance among customers who utilize e-commerce services. This indicates that as many as 400 million Indians already have experience utilizing healthcare services. Specifically in the case of online pharmacies, experiential similarity vis-à-vis e-shopping and online retail have helped them to deeply penetrate in the telehealth space. The survey found lower traction in e-diagnostics, which is understood to be due to perceived lower quality and accuracy of diagnoses, patient desire not to interfere with physician recommendations, and the facility operations (turnaround time, reputation, etc.). In addition, a clear divide is visible among the key age groups in the acceptance of digital health tools, with those over 40 being about a third less likely to use digital tools than younger consumers, largely because of familiarity and tool awareness among the younger population (see Figure 4). The opportunities do remain relevant for this segment, however, as increases in routine health examinations and lifestyle ailments begin to emerge among the population in the 41- to 50-year age bracket.
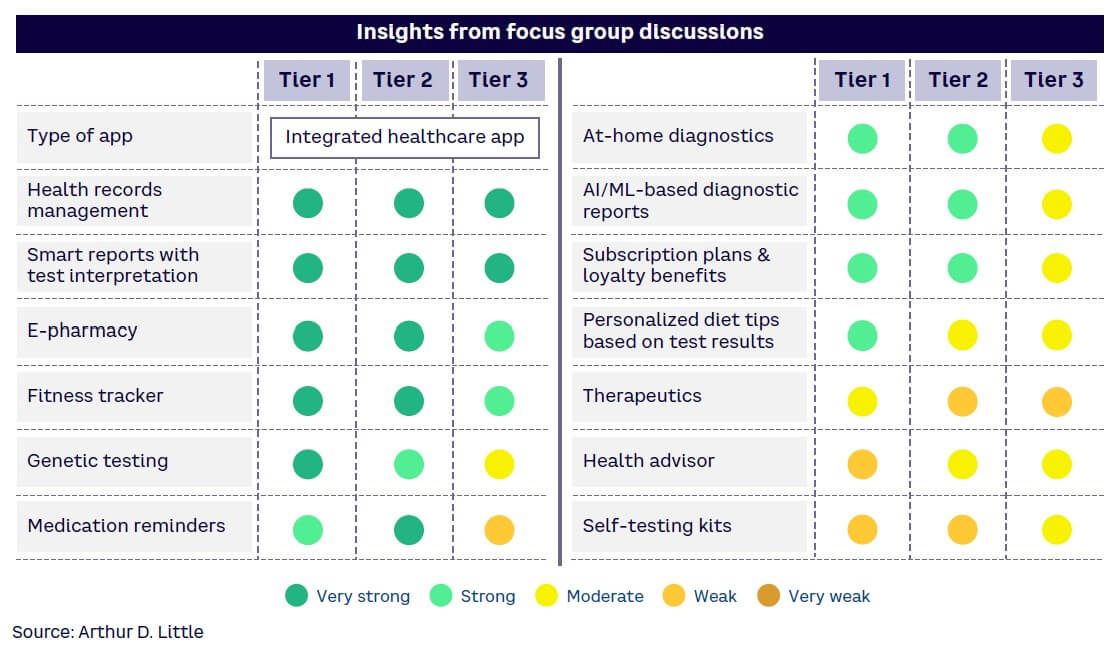
- Larger, more evident value pools in Tier 2 and 3 cities. Except for adoption of e-diagnostics and online pharmacies, which vary somewhat, all tiers of cities have a comparable degree of adoption for digital services, indicating that the technology divide prevalent in the past is now abating (see Figure 5). Tier 2 and 3 customers are also becoming increasingly aware of the benefits of digital technologies in healthcare and are demanding conveniences from digital health offerings.
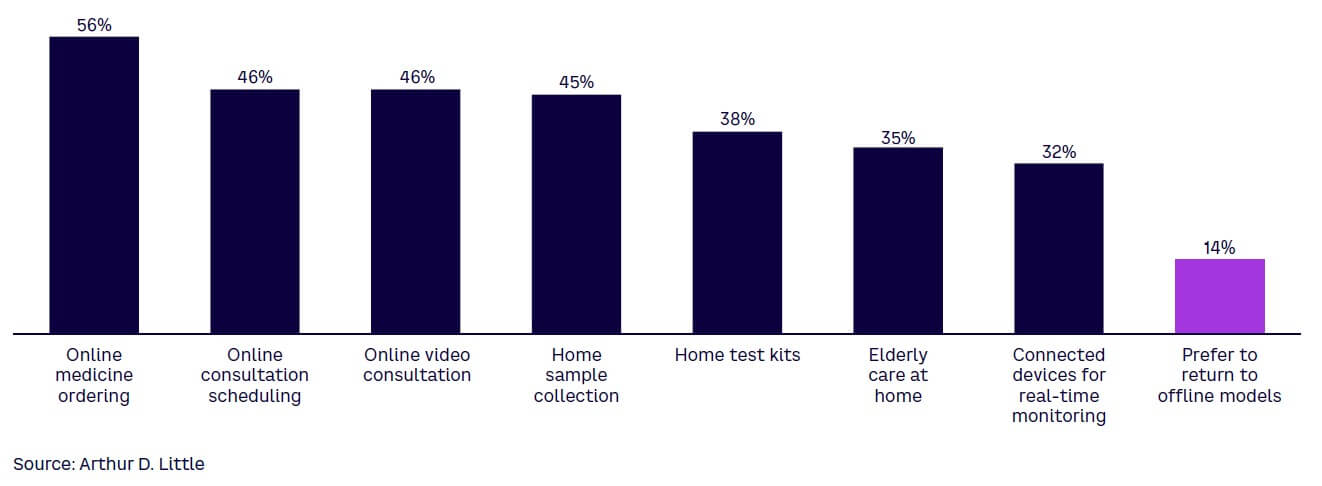
- Stickiness is high among patients using digital healthcare services. Patients who had long-term disorders/ailments such as cardiovascular disease, diabetes, hypertension, or allied indications reported significantly higher adoption of digital health tools (see Figure 6). These patients tend to use healthcare services more regularly and in a more organized manner. As these patients adopt digital healthcare solutions and appreciate their value, they will utilize platforms even more. Digital health solutions must therefore target greater usage of digital tools and track the value of health information communicated to the consumer pool. While patients with chronic illnesses do appear to have a higher degree of adoption of digital health tools, COVID appears to have catalyzed sustained use of digital healthcare tools in India (see Figure 7). Patients were initially compelled to utilize digital channels for care needs due to movement restrictions and infection risks. However, once they experienced the benefits of digitally enabled healthcare delivery, these are now increasingly considered as necessities. It is no surprise that only ~14% of respondents accustomed to using digital health services indicated a preference to return to offline modes for health.
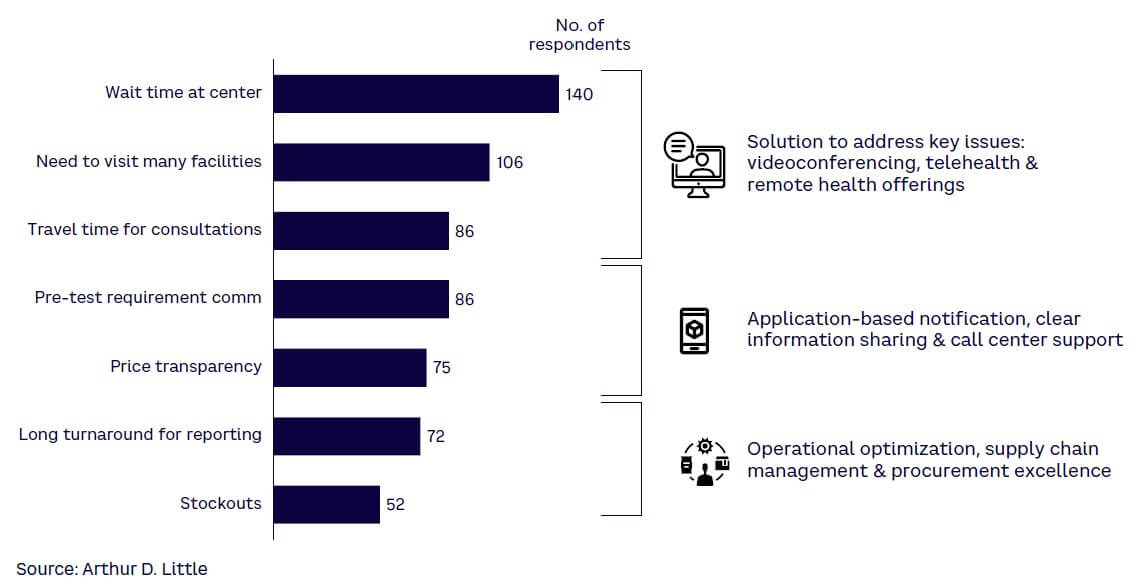
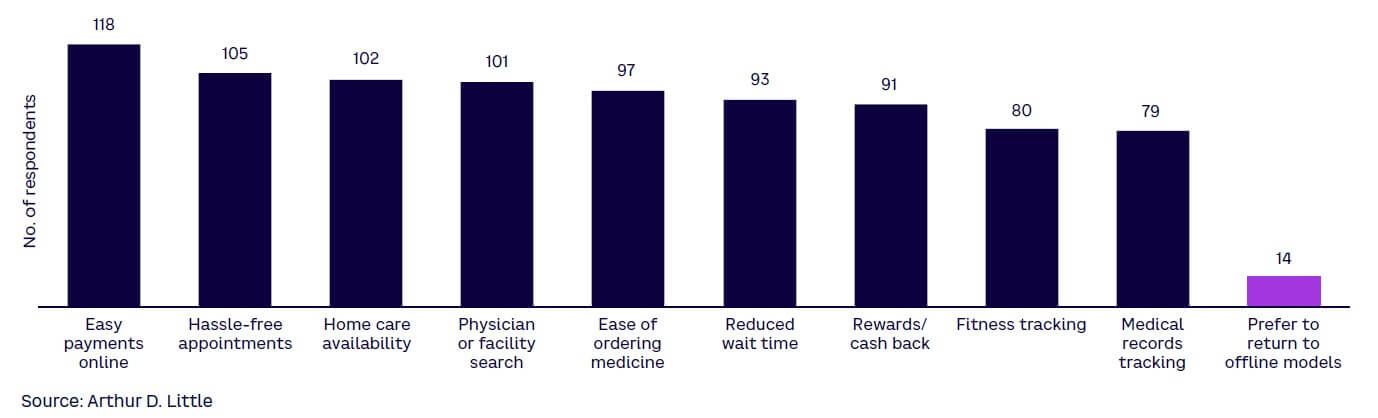
- Seamless integration across the consumer journey is critical for success. Key pain points for consumers remain in the brick-and-mortar components of health (see Figure 8). Many of these can potentially be resolved through digital health offerings, but only if there is a deeper integration of tech solutions with brick-and-mortar care delivery. Physical interactions — if minimized either through implementation of videoconferencing, telehealth, or remote healthcare solutions, or through application-based updating and support, or through operational transformation to ensure ready access to findings and medical supplies — can help in improved uptake and easier access to patients (see Figure 9). In addition to the above pain points, several experiential and non-transactional aspects of digital care delivery are important for customers.
- A preference for integrated applications that provide the whole spectrum of healthcare offerings. Consumers reported that applications that provide several healthcare services along with the option of storing health records are preferred (see Figure 10).
5
DIGITAL HEALTH OPPORTUNITIES IN INDIA
The case for at-scale digital adoption in India
The Indian healthcare system faces several structural and strategic challenges that create opportunities for novel and innovative healthcare solutions. India’s healthcare capacity — in terms of infrastructural capacity and caregiver coverage — remains behind regional and international benchmarks for both.
For example, in terms of bed density, or the number of beds per 1,000 people, India currently ranks lower than international benchmarks as well as most regional economies (see Figure 11). This is compounded by the fact that in Tier 2 and 3 cities and beyond, healthcare systems and access are significantly challenged and undersupplied.
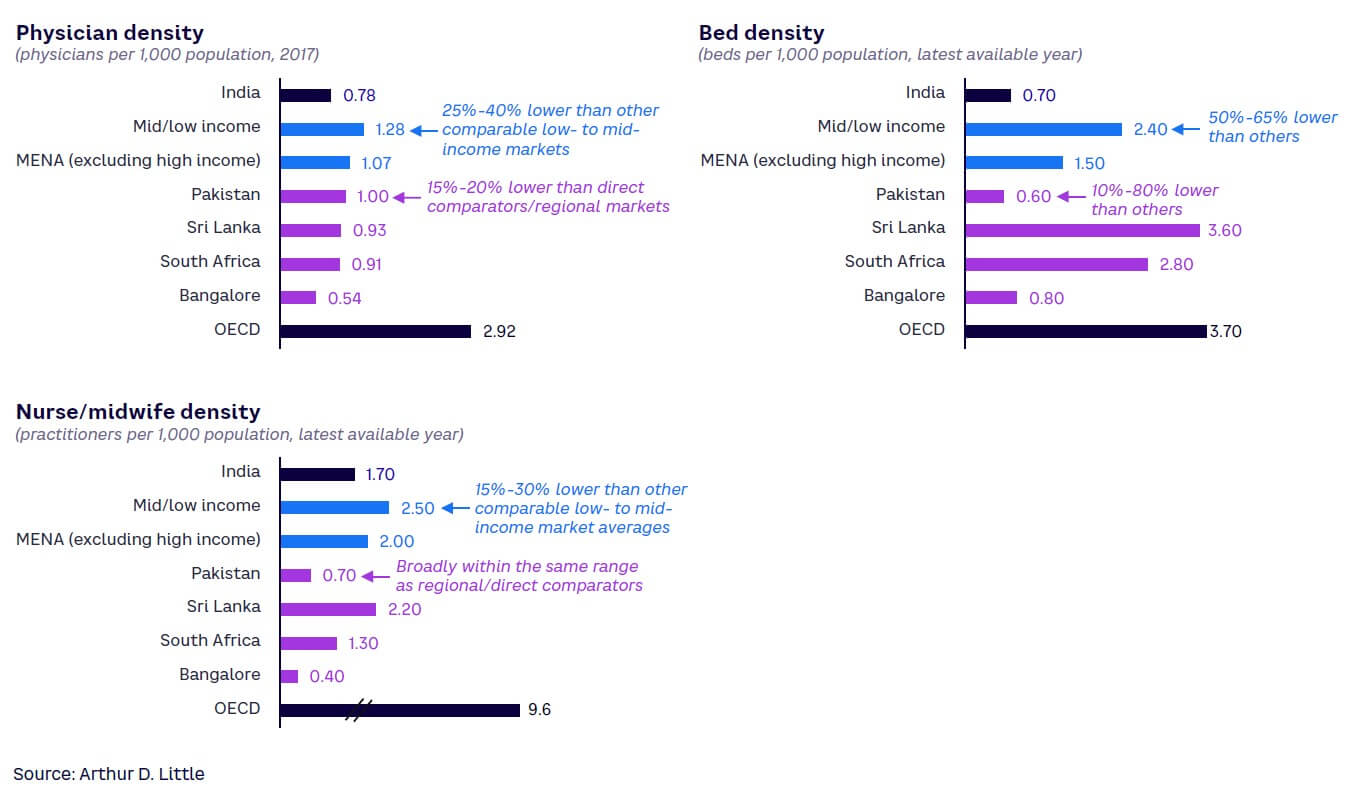
From a care delivery staff perspective as well, India is largely under-resourced to deliver care to its citizens compared to international as well as regional benchmarks. Plugging these gaps conventionally may require incrementally training and developing thousands of physicians, nurses/midwives, and other clinical staff, likely a herculean challenge given the time required to educate, train, and nurture a high-performing healthcare practitioner and the limitations that exist in health education infrastructure in the country.
At the same time, from the perspective of utility infrastructure (power and water access, etc.), telecommunications infrastructure deployment, and information access, India has made significant strides in the recent past — creating an effective foundation for digital health platforms and solutions. In fact, India now boasts the second-largest number of cell phones anywhere in the world, and smart device penetration stood at about 54% in 2020, up from only 22% in 2016.[4] With omnipresence of low-cost smart devices, penetration is expected to reach near full saturation by 2030-2035. India also had among the highest data usage globally, at about 12 GB per month per user in 2020, a number that is expected to double by 2025.[5] As 5G network access becomes accessible to urban centers, the digital revolution in healthcare will have an effective connectivity backbone.
Potential impact of ABDM deployment
In addition to infrastructure and connectivity-related interventions that have progressed rapidly in recent years, healthcare policy in India has also been aimed at creating a foundation for digital healthcare innovation through the Ayushman Bharat Digital Mission (ABDM) program. ABDM primarily aims to improve the quality and knowledge base of India’s healthcare sector in a consistent, unified, and standardized manner.
The ABDM program is critically important to affect a step change in digital health platforms. With a primary objective to establish a health data capture framework, the program can support the eventual development of a “single source of truth” for personal- and facility-level health data across the entire population of India.
The core of the ABDM program is the Unified Health Interface (UHI) framework. Reliable sources of data and leveraging that data to analyze performance and drive improvement are critical to supporting and sustaining an eventual insurance-covered healthcare model.
As information travels across the continuum of care, it becomes difficult to measure healthcare quality and facility performance. The UHI is targeted at providing a consistent data foundation that delivers actionable information to all health stakeholders and policy makers from a consolidation of various data sources. The UHI is envisioned to:
- Streamline the digital health service experience for providers and patients by establishing and standardizing the technology pathways that enable such services to be given.
- Provide an open protocol for various digital health services, including a UHI Network, an open network of end-user applications (EUAs) and participating health service provider (HSP) applications.
- Enable interoperable connections over a nationwide decentralized, open, secure, and inclusive network, using ABDM registries that keep a list of the entities participating in the network and utilize gateways that enable communication using standard protocols.
Ensuring safe storage and easy access of medical records and access to accurate information on healthcare providers will allow better decision making by the Indian government. Geography- and demography-based monitoring and effective evaluation of various programs and interventions will enable the government to adjust depending on patient outcomes.
The overall architecture of the program includes a four-layered structure:
- A unique identification database that includes public digital goods such as the Aadhaar unique identification number for patients, facility registry for hospitals, and professionals registry for practitioners.
- The collection and maintenance of health data at the patient, practitioner, and facility levels.
- A unified health interface to enable consistent and secure access to relevant health information.
- User applications such as the COVID-19 tracker Aarogya Setu and other cases to deploy solutions that accept information from the UHI layer.
The program, upon full implementation, has the potential to realize several benefits to stakeholders across the healthcare ecosystem. For key participants, there may be several opportunities:
- Patients — a singular and consistent clinical history will enable better diagnosis and comorbidity management, easier case reviews and second opinions, better availability of health data resulting in diversified and lower health premiums, reduced transaction time and costs for health insurance, and systematic tracking of health progress.
- Healthcare professionals — collecting standardized and unified health information will enable better clinical decision making, greater data availability for patient treatment, better and easier assessment of clinical risks, and easier and more streamlined clinical protocol monitoring.
- Healthcare providers — enabling community partnerships, easier linkage with governmental and social programs as they get deployed, greater access to patient pools, better clinical risk monitoring, better morbidity management/tracking, and enhancing competitiveness vis-à-vis other market participants. Effective data use can also enable catchment expansion for high-quality and efficient facilities as well as reduced marketing and patient outreach costs, resulting in increased visibility of the hospitals’ doctors.
- Health insurers — optimizing the insurance lifecycle, as adopting the health ID as a patient ID could enable consent-based access to linked health records. Opportunities exist as well in policy portability and information exchange, allowing patients to link a single health ID to multiple provider and insurance IDs for cross-insurer consistency checks and fraud prevention. Policy premiums may also be optimized for lower-risk/healthier individuals, and more diversified and larger risk pools may be enabled.
- Researchers — enabling clinical variations for enhancement in care pathways, new product development, clinical trials management and selection, and outcomes enhancement.
- Policy makers — effective capacity tracking and monitoring, surge capacity management, and redirection of policy initiatives toward emerging areas of lacunae.
Opportunities for digital health across care continuum
The opportunities that arise with ABDM have the potential to make healthcare delivery in India much easier and faster by leveraging information and communication technology. Given the market gaps and digital access enablement for external solutions, coverage and capability improvement measures may represent significant growth opportunities in the Indian marketplace. Use cases that likely will gain traction in the market center around:
- Digitally enabled home healthcare, chronic care, and extended care. Home healthcare for chronic diseases and lifestyle ailments may offer potential for digital enhancement. Patients and families of patients have historically relied on fragmented and unstructured recruitment of home healthcare practitioners through personal networks, regional ads, and so on. Aging and life expectancy increases have resulted in a rise in clinical care being provided in a home setting. These services potentially can be aggregated and provided in a bundled format at home.
Several use cases emerge in geriatric care and home healthcare involving the use of IoT and wearable devices. For example, GPS devices that track and monitor patients may be affixed to a patient’s clothing or person to assist caretakers in cases of patients with cognition challenges. Geofencing can also be used to alert caregivers to patients who leave or cross certain thresholds or boundaries. Tracking patients on an active basis allows patients freedom in movement within and outside facilities while retaining the ability for caregivers to find and assist in case of an emergency.
Wireless home-monitoring technology solutions are also becoming increasingly mainstream as streaming video devices become more miniaturized, energy efficient, and better networked even in markets with lower disposable incomes such as in India. These technologies allow caregivers to identify and monitor patient behavior and in-home appliance usage to minimize risks associated with injuries, enabling greater household safety and speedier response in case of adverse events.
- Preventative care enabled through IoT devices. Wearable sensor technology to track routine activities such as walking patterns, location and positioning, fall/injury detection, emergency messaging/SOS, and heart rate or vitals monitoring also enables caregivers to provide and extend care to larger patient pools while also providing more customized care and monitoring of specific cases. IoT devices are becoming increasingly affordable — particularly wearables — and are gaining traction among the population, with wearables alone registering growth of 93.8% by volume, according to India Brand Equity Foundation (IBEF). Large market shares are being captured by value segment players like Noise, boAt, Realme, and other players launching products in the affordable INR 3,500-6,000 range. Collected data from sensors over a period — if collected in a platform approach — can be used for preventative care rather than responsive care as well.
- Electronic medical record (EMR) adoption and diagnostic data integration. EMR adoption is the next digital frontier in Indian healthcare, primarily driven by the ABDM. The next wave of growth in medical data generated from health information systems is catalyzing the next iteration of care delivery — utilizing big data and evidence-based care and applying these principles to enable:
- Precision medicine — utilizing research and centralized data to promote enhanced diagnostics and personalized patient care.
- Safety practices — use of predictive analytics to promote quality care and patient safety (e.g., infection risk monitoring).
- Population health management — utilizing analytics in epidemiology (e.g., linking EMRs with GIS to identify healthcare trends in specific areas).
- Readmission analytics — analyzing EMRs to reveal trends that highlight patients likely to need additional treatment to prevent readmission.
- Data security — securing medical records by identifying changes in network traffic or behavior that indicates a cyberattack.
- Insurance claims — improving the efficiency of medical insurance claims by revealing claim trends and streamlining claims processing.
- Consistency and standardization in data being collected from diagnostics can also allow longitudinal tracking of key biomarkers.
- Tech-enabled capacity augmentation. Concepts such as e-ICUs and virtual hospitals (some of which are already under pilot deployment with start-ups/large healthcare groups) enable efficient deployment of critically scarce intensivists while also enabling asset-light operations in the conventional healthcare delivery approach. e-ICUs and virtual hospitals may allow several advantages over conventional facilities, including lower headcounts (on a per patient served basis) for highly trained and skilled intensivists, reduced risk of nosocomial infections due to lower contact, reduced hard CAPEX cost in real estate components of healthcare provisioning, and superior distribution of super-specialty intensivists’ capabilities across a wider group of healthcare facilities or geographical centers.[6] Consultations in India represent another digital opportunity — both for primary care visits as well as post-care follow-up discussions. India is also a significant healthcare destination from a Medical Value Travel (MVT, meaning travel in pursuit of healthcare) perspective. Historically, India’s positioning as an MVT destination has been largely on account of the high quality and deep experience of physicians practicing in the marketplace, significantly cheaper cost of care on a dollar-to-rupee basis, and the soft-power presence of India as a nation, with the capacity to advance foreign policy objectives and priorities through noncoercive means. Opportunities exist for digital health to provide pre- and post-procedure support through digital offerings.
- Scalable supply chain and aggregated value-based procurement solutions. Healthcare provider networks in India straddle a large spectrum of capability areas and sizes — from single-facility family-owned healthcare organizations to integrated and broad-based chains with dozens of hospitals operating thousands of beds across multiple cities. Smaller players represent opportunities to aggregate supply chain services under a data- and digitally enabled umbrella.
- Predictive/prescriptive digital supply chain management solutions. For large-scale players, standardization is a critical factor enabled by digital offerings. Processes, such as procurement of any materials, their management, and tracking, need to be made consistent across network/s. A universal approach leads to effective supply chain and vendor management as systems move to a central procurement management model across the entire spectrum of supplies. A digital health use case that may be deployed at scale is predicting the nature and amount of stock moving at a certain point of time, based on historical demand/supply data. Automating procurement functions and configuring reorder levels, inventory levels, reserves, and stock-out levels can all be optimized through effective use of digital offerings. Value-based procurement can be enabled through use of analytics and big data. Such systems, if executed well, can also provide necessary checks from a supply chain governance perspective. In addition, systematic tracking to prevent pilferage and misuse of items can lead to significant revenue losses. Systems should also be integrated in the financial systems, such as invoicing and digital payments. Integration and automation of supplier reviews and consolidation of supply also supports the maintenance of relationships with vendors and suppliers.
- AR/VR-based training in specialized care. AR/VR-based applications represent opportunities for a variety of training and capability development sessions. For low-complexity physician education programs by pharma and medical devices companies, pure AR/VR solutions may suffice. However, for more technically complex medical devices/implant-based training and development activities, mixed-reality applications are also emerging — reducing the training gap by enabling physicians and care givers to gain tactile experience in addition to audiovisual experiences.
- Digitally enabled aggregation for standalone facilities. A large majority of India’s healthcare system is disaggregated and consists of standalone facilities. These facilities may not have the scale to reap benefits from digital health enhancements even if they choose to invest. Capabilities to effectively deploy effective and integrated digital health solutions in these facilities may also be a constraint in a large majority of such facilities. Nor will it be easy for smaller facilities to comply with or leverage the unified health information structures that will be rolled out under the ABDM program. This represents a clear opportunity for health tech enterprises to develop modular, scalable, customizable, and easily implementable solutions for such players. Similar opportunities also exist in digitally enabled supply chains and procurement value creation initiatives. Standalone facilities may have demand variabilities and challenges in integrating digitally with suppliers. These facilities may not have the right capability set to push value-based procurements concepts viably. However, intermediaries who can aggregate and can digitally interface with both suppliers and consumers can potentially facilitate the process, offering predictability, managing economic order quantities, and enabling efficiencies in procurement.
- Medium- to long-term opportunities. In addition, several other opportunities can be digitally enabled and made more effective. For example, digital loans, with funding linked to clearly defined digital readiness and easier financing access, can allow health organizations to invest in digital and improve their “digital internal rate of return.” However, this may require the digital health ecosystem in India to become more formalized and for digital health players to become more standardized and segregated. As digital penetration starts to hit critical mass, the middle- and lower-income segments in India will also start to become viable from a service-delivery perspective. These segments already have growing penetration of smart devices and platforms to support digital health. With increasing availability and critical mass, the fortune at the bottom of the healthcare pyramid in India can become digitally accessible as well.
Over the longer term, as the overall health delivery system matures, India may move toward coordinated health, and eventually toward a managed health network. However, this will require the entire ecosystem to be able to exchange information on a common framework — something that will be enabled through digital health offerings.
CONCLUSION
11 IMPERATIVES FOR INDIAN HEALTHCARE ECOSYSTEM
India presents a unique opportunity for an existing digital health user community of 400 million people. With the further penetration of smartphones, 5G adoption, and service provider innovation, by 2030 India could easily have over 1 billion digital health users. This will help catalyze a transformation in Indian healthcare, creating the platform to provide quality, affordable care to all Indians. The government has also created a scalable technology architecture (through the ABDM) for healthcare ecosystem players to drive technology-led transformation of the sector. The healthcare industry now needs to step up and break through the digital divide. To realize the full potential of digital health, we propose the following imperatives for the various industry stakeholders.
Provider imperatives
Providers remain the foremost point of interaction between end users and health systems. While COVID has accelerated the digital uptake and improved accessibility, a lot of providers look at digital to be another business unit rather than a force multiplier. Providers must ensure integration of digital systems within the provider space and other stakeholders to enable meaningful digital changes and use of digital first as a strategic advantage:
- Digital first. Providers face a risk of getting disrupted by digital interventions, entrepreneurs, and competitors unless they have a digital-first strategic outlook. It is essential that they create deeply integrated offerings to capture and retain the consumer base over the long term. At the same time, digital should not just be considered as a front-end/patient interface activity and should be cost effective and focused to capture efficiency gains. At the same time, emphasis should be on building digitally enabled supply chains that are resilient, scalable, and efficient.
- Platform offerings. Healthcare offerings have specialized and moved beyond the confines of hospitals. A variety of services and products are home-based, hospice-based, or can be used anytime/anywhere. To improve customer loyalty and stickiness, it is essential that product and service availability be improved through a platform approach. This would require providers to partner with each other, payers, and other stakeholders to create meaningful health service platforms.
- Partnership strategy. The rising complexity and scale-up challenges of digital product development make it imperative that providers do not build everything and instead try to reduce the risk of failure. Build-buy-develop decisions and consequent actions are vital. A provider must have a strategic need-solution analysis framework and an ecosystem that helps them to integrate multiple products easily. This must also be reflected in operations, strategy, human resources, and advisory capabilities.
- Data strategy. With the advent of digital capabilities, providers are required to collect, manage, and store large amounts of data. This data can provide intelligence to personalize offerings and improve customer stickiness, but it requires a detailed digital data strategy to ensure the organization uses the data within the confines of regulations and privacy. Providers may develop the data strategy along with offerings to comply with regulations while utilizing the multiple benefits of healthcare data.
Payor imperatives
Healthcare payers have traditionally dealt with a fragmented ecosystem, which has resulted in multiple redundant systems to distribute products, process claims, and reduce fraud. Digital products can solve these redundancies by reducing the cost of acquisition and improving the efficiency and effectiveness of claims processing. The ecosystem needs products that can solve for both the payor and end customer while ensuring seamless integration with provider systems:
- Digital insurance distribution. The penetration of insurance products in India is poor, and few start-ups and digital disruptors have taken up the opportunity to digitize distribution, posing serious challenges to existing players. Payors must identify the opportunity, develop digital distribution platforms, and partner with providers and other stakeholders to enable digital transformation in their business. This would entail developing a strategic vision in developing the offering while ensuring customer focus and ease.
- Health claims platforms. Rising healthcare complexity — with instances of fraud, misrepresentation, and increases in volume — exposes payors to financial and operational risks. This can be mitigated by integrated health claims platforms with claim, disbursal, fraud detection, and analytics with minimum human effort and cost. Providers must have a strategy toward development and deployment of the claim platform and integration with providers, distribution, and regulators to ensure low risk and higher efficiency.
Regulatory imperatives
While regulators and policy makers have taken steps in the right direction, they will also need to become the system’s conscience as digital offerings are rolled out. The most critical imperative for policy makers will be to ensure the program is governed effectively and appropriately. Data access, availability, and privacy are concerns of global consequence and, with greater consumer awareness, it will be necessary for regulators to be the custodians of the health data that is generated:
- Regulatory framework. Being an ombudsman looking to balance compliance with the prescribed standards and commercial and policy support considerations.
- Start-ups. Supporting new and incumbent digital players to garner and secure funding for health tech start-ups.
Investor imperatives
Investors remain the key accelerating force in every industry, and that is no different in digital uptake in healthcare. Investors have always welcomed digital offerings and solutions to improve efficiency and margins. However, investors must undertake systemic changes to ensure digital products in healthcare are integrated, drive enhancements in the health system, and reach the end users for whom they have been designed. These changes include:
- Targeted digital financing. As the start-up ecosystem and linked investor base start to deploy resources aggressively in new product and service line development and new ventures targeting digital health opportunities, an attractive and independent ecosystem could gradually emerge supporting digital-first offerings. These will need to be nurtured and effectively managed by the investor group while ensuring digital ability is considered as integral in deal flow and screening processes, and not just an incremental differentiator. In parallel, the start-up ecosystem must integrate and penetrate brick-and-mortar healthcare delivery to enable access to care.
- Driving true integration. A digital-first investment/resource allocation approach should not become a “digital only” approach for investors and health tech start-ups. True integration is only possible with both the digital and brick-and-mortar realms being seamlessly integrated. Ensuring investment/M&A targets will need to be screened and scored with a quantitative approach. All of these should be targeted at developing an attractive, independent, and lucrative investment ecosystem for investment in health, health tech, or digital health trends. Digital health should also be considered by investment houses during the deal evaluation, deal assessment, and, eventually, a value creation plan.
- Novel financing areas. Investors need to finance digital health innovations and platforms through greater emphasis on health tech and insurtech start-up ecosystems. This would enable growth of the entire ecosystem and add value to innovators and disruptors.
India stands at the cusp of a revolution in healthcare access, with several public healthcare schemes as well as increased private interest in healthcare delivery. Digital remains the most potent force multiplier to enable a mature and efficient health system. These 11 imperatives are key to unlocking value while moving to a digital-first healthcare system and ensuring that the system is integrated, efficient, and has participation from all stakeholders.
Notes
[1] “Noncommunicable Diseases.” World Health Organization, 16 September 2022.
[2] “2022 World Population by Country.” World Population Review, accessed October 2022.
[3] “Medical Devices Market — Growth, Trends, COVID-19 Impact, and Forecast (2022-2027).” Mordor Intelligence, August 2022.
[4] “Smartphone Penetration Rate in India from 2010 to 2020, with Estimates Until 2040.” Statista, accessed October 2022.
[5] “Average Data Consumption per User per Month in India from 2015 to 2021.” Statista, accessed October 2022.
[6] Iyengar, Karthikeyan P., et al. “Electronic Intensive Care Unit: A Perspective Amid the COVID-19 Era — Need of the Day!” Lung India: Official Organ of Indian Chest Society, Vol. 38, Supplement, 2021.
DOWNLOAD THE FULL REPORT
37 min read • Healthcare & life sciences
A bold vision for India’s digital health
A digital revolution driven by the Indian consumer awaits
DATE
FOREWORD
Across the healthcare spectrum, technological innovations continue to be developed and made available to consumers at breakneck speed. Within this evolving healthcare landscape, care is becoming more personal, more patient centric, less episodic, more omnipresent, and fully embedded in the lifestyles of the population. Innovative use of digital technologies therefore creates opportunities to enhance patient experience and at the same time optimize care delivery to ensure affordable health access to all. Resulting changes in the fundamentals of healthcare delivery affect all components of the healthcare value chain — from outpatient care enabled through telemedicine, to inpatient care optimized through remote care and home health enabled through digitalization, Internet of Things (IoT), and other interventions.
The COVID-19 pandemic has catalyzed both technological and behavioral change — on one hand, forcing people to embrace digital innovations in all areas of life and especially healthcare, and on the other, creating significant pressure on health systems and exposing supply chain lacunae globally. As a large and growing healthcare market and a hub for innovation and digital entrepreneurship globally, India is poised to see a paradigm shift in digitally enabled healthcare. In this context, this Report seeks to explore how global trends and success stories in digital health will be relevant in the Indian context, what opportunities could emerge in the near future, how ready the ecosystem is to adapt to the changing landscape, how recent policy interventions have set the stage for accelerated adoption of digital health, as well as what specific challenges may need to be overcome and how these translate into innovation opportunities for Indian healthcare players.
- Barnik Chitran Maitra, Managing Partner, ADL India & South Asia
- Shravan Subramanyam, President, NATHEALTH, CEO, GE Healthcare
- Siddhartha Bhattacharya, Secretary General, NATHEALTH
- Vikas Kharbanda, Partner, Healthcare & Life Sciences, ADL Middle East
EXECUTIVE SUMMARY
Digital technology has a transformative power that eclipses the capacity of any other force behind earlier socioeconomic revolutions. In healthcare, digital technology is creating a quantum shift, one that could transform healthcare in India almost beyond imagination. India could have 1 billion digital health users by 2030, enjoying an inclusive health system where healthcare keeps expanding but costs keep falling — a system that efficiently prevents and treats diseases and responds to individual lifestyles and disease profiles with tailored treatments, all at an affordable price.
This is a future that the digitization of healthcare can achieve. But only if the stakeholders involved step up to the challenge.
The demand already exists. India already has 400 million digital health users, using available services such as telehealth, home health, home testing, e-pharmacies, and other digitally powered offerings, even without much innovation by large healthcare providers. A survey by Arthur D. Little (ADL) to identify what drives digitized healthcare adoption in India showed up to 65% acceptance of digital health solutions among customers who use e-commerce services. Significantly higher adoption of digital health tools was reported by patients who had long-term disorders such as cardiovascular disease, diabetes, and hypertension. The pandemic forced people to use digital channels for care needs. Having experienced the benefits of digitally enabled healthcare delivery, consumers now consider them a necessity.
However, as too often in India, supply lags well behind demand. The underpinnings are already there — India now has a sturdy digital backbone via Ayushman Bharat Digital Mission (ABDM). Aiming to capture health data across physicians, providers, and patients, the platform promises interoperability, flexibility, security, scalability, and wide access.
It is now up to healthcare providers, start-ups, technology providers, investors, and other stakeholders to develop digital health offerings that meet and stimulate demand. Like nature, the economy abhors a vacuum — those who tarry could find that others have already captured the opportunities.
At the moment, opportunities abound. What India needs is effective, accessible, and high-quality healthcare solutions that provide equitable access and that can be rapidly deployed and scaled up. Conventional healthcare capacity is highly unlikely to catch up with the demand and supply gaps the country suffers now. Digital solutions are the answer, building on the deep penetration of smart devices and increases in connectivity that the country has invested in over the past decades.
The pandemic catalyzed the adoption of telehealth, home health, home testing, e-pharmacies, and other digital offerings. But there is still a lot of room for growth. Meanwhile, some solutions remain largely unexplored, including e-diagnosis and tech-enabled home health and more mature e-pharmacy solutions.
For conventional healthcare players, health technology start-ups, and investors, this is the time to enter and build a hard-to-beat position. How they could do so and the policy and regulatory support they will need can be summarized as follows across 11 imperatives:
Provider imperatives
- Develop “digital first” strategies instead of “digital as a bolt-on” for conventional businesses.
- Create digital health offerings that are integrated — from preventative health to patient first contact to point-of-care delivery, onward to post-care follow-up and then recuperative care.
- Orchestrate partnerships and build-buy partner strategy.
- Set a clear data strategy to use data to improve the health system.
Payer imperatives
- Develop digital distribution strategies focusing on customer ease and accessibility.
- Build health claims platforms to improve efficiency and reduce risks and fraud.
Regulatory imperatives
- Develop regulatory framework for policy that pushes legacy players toward adopting digital health offerings while providing trust in digital solutions, data security, and consumer satisfaction.
- Encourage start-ups through the right regulatory and policy support.
Investor & funding imperatives
- Develop an attractive, independent investment ecosystem for digital-first healthcare plays as opposed to digital health investments — with digital as a key parameter for investment ideation, deal identification, transaction screening, and post-deal value creation.
- Start targeting brick-and-mortar services from an integration perspective where some momentum is already observed (notably with large players like Practo and Pristyn Care).
- Finance digital health innovations and platforms through greater emphasis on healthtech and insurtech start-up ecosystems.
1
GLOBAL HEALTH TECH ADOPTION TRENDS & DELIVERY INNOVATIONS
Key trends impacting healthcare sector
The future of healthcare is being shaped by several trends. Fundamental shifts in demand and epidemiological characteristics, demographic and access improvement in healthcare, emphasis on supply chain resilience, changing consumer preferences and views on healthcare, increasing automation, standardization, and efficiency are driving the evolution of the healthcare sector as well as digital health and health tech innovation.
Globally, noncommunicable diseases (NCDs) are expected to drive a lion’s share of disease burdens, according to the World Health Organization.[1] NCDs are already the leading cause of mortality and disease burdens globally, contributing to over 70% of deaths globally before the COVID-19 pandemic. The shift has already permeated from developed countries to developing countries and notably India as well. As many as 77% of NCD deaths globally now occur in developing countries like India. Key ailments like cardiovascular diseases, cancers, respiratory diseases, and metabolic disorders drive a majority of the mortality burden in India as well.
Notwithstanding the impact of COVID-19 in the short term, comorbidities and risk factors such as diabetes, hypertension, and cardiovascular susceptibility are well known to have driven significantly higher mortality among vulnerable patient groups during the pandemic as well.
As life expectancy increases globally, and especially so in developing markets, the need for healthcare services is expected to increase significantly as well. In fact, the expected increase in the proportion of people above the age of 60 is set to grow 1.5 times over the next 20 years (14% in 2021 to 20% in 2040).[2] Access to better healthcare must improve at the same time to enable a healthy population to thrive and grow.
During this period, the elderly population (those people older than 80 years old) is likely to grow from about 125 million globally to over 434 million by 2050, with sizable growth in this demographic being contributed to by large and (currently) developing markets like India. Public health agencies and experts also suggest that the incidence of long-term ailments and chronic conditions such as dementia and Alzheimer’s will continue to grow. Estimates point to an increase of this incidence from 47 million in 2015 to 75 million by 2030.
Demand for this demographic segment currently has larger scale in developed countries with older demographic bases. However, as the populations in developing countries age further, the younger population ages, and fertility rates stabilize, developing economies can also expect to see the elderly segment becoming increasingly critical.
Healthcare delivery paradigm shift
As the need profile evolves, the care delivery approach to address the demand is also evolving. All dimensions of the care delivery paradigm are being impacted — from overall targeted objectives and design criteria for the healthcare ecosystem, to focus of treatment, service delivery approaches, novel care delivery settings for optimization, shifting accountabilities of health outcomes from physicians to a collaborative approach with patients, to funding of health systems on activity basis to an outcomes/outputs basis (see Figure 1).
The emerging paradigm will force care delivery models to go beyond just delivering care outside the provider infrastructure and start to make healthcare more omnipresent with the health consumer. Specifically in an Indian context, care delivery models need to also evolve and create more equitable and democratic access — servicing the marginalized and at-risk population groups more effectively. Tech-enabled business models in healthcare therefore likely need to be rethought to create infrastructure and service offerings designed for such delivery modalities.
2
GLOBAL TRENDS IN DIGITAL HEALTH & ENABLEMENT
Technology-enabled change in the healthcare space has also seen significant acceleration in recent years, especially from the perspective of development of new treatment modalities and changes in clinical methods. Even traditional areas of technological adoption have seen significant and rapid growth. New vaccine developments are a benchmark example of effective technological adoption in fundamental healthcare delivery. Complex vaccine development activities, typically taking years or decades, have been accelerated to be completed in months due in large part to technological advances in genomic sequencing, collaborative research with leading universities and research programs, and rapid scale-up of technological offerings.
Shift from information digitalization to digital health
Use cases of digital technologies in healthcare target a shift in the way information is received and processed in the healthcare system. The emphasis of emerging, scale-based solutions is to move away from pure digitalization of information toward developing digital solutions in care delivery.
Health data, at the same time, is diverse and collected across a variety of platforms in a complex healthcare ecosystem. Systemic sources of information could be supplemented by data and interpretation of physical testing/diagnosis.
The diversity and lack of unified structure in collected information represents challenges that can be addressed at scale. Connecting collected data from patients and filtering relevant information for clinical decision making is critical for efficient and effective care delivery. Additionally, the availability of standardized, curated, and accurate information regarding patient demographics, health history, prior complications, comorbidity status, and severity are all critical decision points that can be integrated for clinical decision making.
Scale-based clinical data collection and standardization can then support health information networks and exchanges that enable research activities such as clinical trials, payor optimization, and transfer of information among different health information systems that may be in large-scale use, in addition to supporting treatment decisions by physicians.
Remote health & virtual care delivery becoming mainstream
With patient care moving away from facility-based treatments to virtual models, ecosystems trending toward maximizing care access to all patient groups, and improving access to telecommunications infrastructure, multiple remote health and virtual care use cases are gaining significant traction globally. These include offerings across the entire spectrum of patient care — from telediagnosis and teleconsultation services, which are lower complexity in overall delivery, to electronic ICUs (e-ICUs) and virtual hospital concepts.
The e-ICU platform is a centralized model in which nurses, doctors, and administrators are connected to one or more satellite ICUs. The platform combines audio/visual technology, predictive analysis, data visualization, and advanced reporting to overcome ICU capacity constraints and extends critical care to patients regardless of their location. Advanced clinical decision support analytics enable providers to intervene at the earliest indication of patient deterioration.
Telemedicine, virtual hospitals, and e-ICU concepts have already seen mainstream traction, catalyzed by COVID-19-related travel restrictions and infection issues. In addition, the use cases for telemedicine concepts also allow for lower-cost/higher-volume countries like India to become referral centers for higher-income, lower-volume countries.
COVID-19: Catalyst of change in digital health
COVID-19 has had a significant impact on the growth of technology and digital solutions across several use cases in healthcare globally. Solutions, including digital tools such as teleconsultations, virtual diagnosis, digitalized mental health support, home testing and report generation, and e-pharmacies have, as a result of the COVID pandemic, become more personalized, cognitive, and integrated within the lives of patients and providers. ADL’s interviews with senior leaders indicate that a large number of the beneficiaries/early adopters of these programs have been patients with chronic ailments with a need for periodic follow-ups and patients who require significant post-acute recuperative care as well as those in vulnerable comorbidity groups.
Potentially scalable consumer use cases
AI/ML-enhanced decision making and automation
A broad set of offerings powered by artificial intelligence (AI)/machine learning (ML) applications in healthcare are gaining traction globally. First, tools that support clinical decision making, diagnostics, laboratory, and other direct care delivery aspects are becoming increasingly automated and diagnostics/lab reviews, decision-making support short of consultations, and other care delivery automation activities are under consideration. Second, AI/ML applications in nontherapeutic interventions in mental health and wellness are also undergoing exploration. Third, AI/ML solutions that automate and enhance routine processes such as coding, logging, case tracking, and documentation activities post procedure are also targeting efficiency- and physician-bandwidth-enhancement opportunities. Natural language processing (NLP) applications through chatbots also enable patient information capture, supporting preliminary self-diagnoses for pre-consultation reporting and pre-diagnosis/lab prep, and can enhance efficiency.
Health personalization
With a shift away from episodic care toward preventative care, personalization of health is becoming a key focus area within the digital health space. Consumers of health services are also more aware than ever before that personalization options for healthcare needs exist in the market. Personalized health solutions can therefore be a critical component of the overall preventative care approach in the market, and gamification and rewards can further be used to help ensure that digital healthcare is embedded in the lifestyles of patients.
Several technological developments, such as miniaturization and acceptance of wearable devices by the population, support adoption of personalized healthcare. As technological maturity remains lower than the levels required to enable clinical interventions through wearable tech, the segment is currently restricted to higher-level health data metrics, as other health sensor technologies become mainstream. Consensus estimates of growth in the wearables segment point to 13%-15% growth over the next five years, with the market volumes set to grow three-fold over the next four to five years, to close to 775 billion devices every year.[3]
AR/VR for training and care delivery
With COVID-19 creating significant travel barriers since 2020 and increasing prevalence of low-latency, high-speed network connectivity worldwide, augmented reality (AR)/virtual reality (VR)-based applications are gaining significant traction. AR/VR-based healthcare training for physicians, specialized technicians, and other clinical delivery staff are becoming increasingly mainstream globally, especially in surgical and other specialized therapy areas where availability of physical trainers may be limited. Mixed reality offerings also can offer not just the audiovisual experience but significant components of tactile feel in several therapy areas. In addition, patient-linked use cases for AR/VR are also likely scalable and appropriate for managing and enhancing functional outcomes in patients with behavioral and developmental disorders.
AI for detecting cardiac conditions
Some clinical conditions such as cardiac arrests and stroke can be effectively prevented with early detection and intervention. AI can be used to analyze data sourced from multiple sources such as wearables, patient checkups, and patient vitals to effectively predict life-threatening events such as cardiac arrests. An AI system has been used in Copenhagen, Denmark, to analyze sounds during emergency calls and alert dispatchers with 92% accuracy.
Home hospitals
Building hospitals entails high CAPEX investments with a long breakeven period. To reduce the CAPEX outflow and provide care nearer to patients, some health systems have experimented with home hospitals. These utilize telemedicine, AI, clinical decision-making software, and remote sensing to connect patients and caregivers. The caregivers are provided with real-time data on the condition of patients and assistance on treatment planning and interventions. Caregivers are also alerted to move patients to a higher care facility if needed. This provides a mix of continuous patient monitoring at a lower cost of delivery of treatment for patients.
Predictive modeling
The COVID-19 crisis illuminated capacity planning and surge flow management challenges at the healthcare system level. As a result, facilities and policy makers now capture large amounts of data — from clinical indications to case progression, geospatial data, and clinical and nonclinical demographic data. Predictive modeling may allow multifactor analysis and identification of growth and evolution patterns in epidemiology to assess capacity requirements on a dynamic basis. For example, electronic medical records are being used to detect patterns and estimate the number of hospital visits, number of patients who would return to the hospital within a given number of hours, length of stay, and so on. Researchers at St. Michael’s Hospital in Toronto, Canada, have developed an algorithm that can predict the number of visitors to the emergency department with 95% accuracy, depending on the day of the week, relationship to major holidays, temperature, and climate.
3
SELECT GLOBAL STUDIES
Digital health offerings are accelerating innovation and are deeply impacting procurement functions in the healthcare sector. Healthcare facilities tend to utilize a wide variety of consumables. In fact, a typical healthcare facility may stock several thousands of medical product types and SKUs within their inventory and include tens to hundreds of thousands of SKUs within their overall formulary for procurement and usage.
These products are also widely varied in their characteristics. For example, storage requirements such as temperature, humidity, lighting, and so on, may vary significantly and have a direct impact on quality of clinical outcomes. Clinical shelf life for products may vary from a few months to a few years. Technological changes to products and delivery mechanisms may change. Product recall and safety management create complexity in supply chain management. Products — from lower-cost, basic medications to high-end, high-valued medical devices to legally controlled substances — need to be procured, stored, managed, and tracked through a unified ecosystem by healthcare enterprises. Critically, from an enterprise-viability perspective, procurement cost and pilferage risks may be high or prohibitive as well, which healthcare organizations need to balance. All these complexities necessitate a responsive, effective, and adaptive supply chain management solution for healthcare players.
Big data and tech-enabled use cases in procurement thereby potentially enable the adoption of value-based procurement opportunities in the healthcare sector.
The Indian market has its unique share of challenges in this context, given the increased need for cost-efficient solutions. Given the lower affordability of healthcare in the country and lower penetration of health insurance among the population base, viability of specific use cases for supply chain management remains a key area to improve accessibility. Leading CTOs/CIOs in India’s healthcare space interviewed by ADL make the case for data-driven and digitally enabled procurement. They also highlight the criticality in six areas:
- Right usage of hard technology for product identification and segregation based on the need for and value of the product versus the investment required to collect information on product stocks/usage.
- Standardization of materials for procurement.
- Effective governance around the supply chain to ensure appropriate usage of materials.
- Genuine integration with financial systems and employing tech platforms at their core.
- Transition planning from nondigital approaches to digital approaches.
- Multidisciplinary team engagement at the solution design phase and training of the workforce to ensure alignment with targeted procurement outcomes.
4
INDIAN DIGITAL HEALTH LANDSCAPE
Key constituents of digital health in India
Most prominent and mature digital health platforms in India have historically targeted enhancement of front-end consumer-facing activities within the care pathways. Penetration of services has largely centered around activities peripheral to core healthcare delivery. Activities such as scheduling of visits and appointments, physician/practitioner identification, home diagnostics/sampling, and case history management have seen traction in the Indian marketplace.
Consumer-facing activities comprise four broad categories of product suites (see Figure 2):
- Integrated health provider applications — covering a wide variety of healthcare activities, including physician selection, appointments, labs and testing, medical records, and other associated core healthcare delivery services. Additional activities in this category that may be provided also include allied services such as claims and payment management, billing, and so on. These applications are developed primarily by large-scale players with significant capacity, geographical outreach, and internal system maturity to support integration of offerings. The targeted value proposition for these applications is to ensure customer “stickiness,” patient relationship management, and long-term convenience for patients — especially for chronic care cases.
- Service-specific health provider applications — including a limited but selective offering of specialized services such as labs, diagnostics, dentistry, and so on, with key services including scheduling, home pickup of samples, and report delivery. The targeted value proposition for these applications is largely to expand outreach and enable wider patient capture on a shorter-term basis.
- Integrated health aggregators — covering a wide variety of services, including consultation scheduling, teleconsultations, lab sampling, diagnostics selection, and so on, but with no/limited support from brick-and-mortar infrastructure under the provider’s own umbrella. The primary focus in this category is to enable differentiation through better information sharing with patients and their family members.
- Service-specific health aggregators — including narrow/niche segments of care delivery, operating as information-sharing platforms with consumers and aggregation within a limited service set.
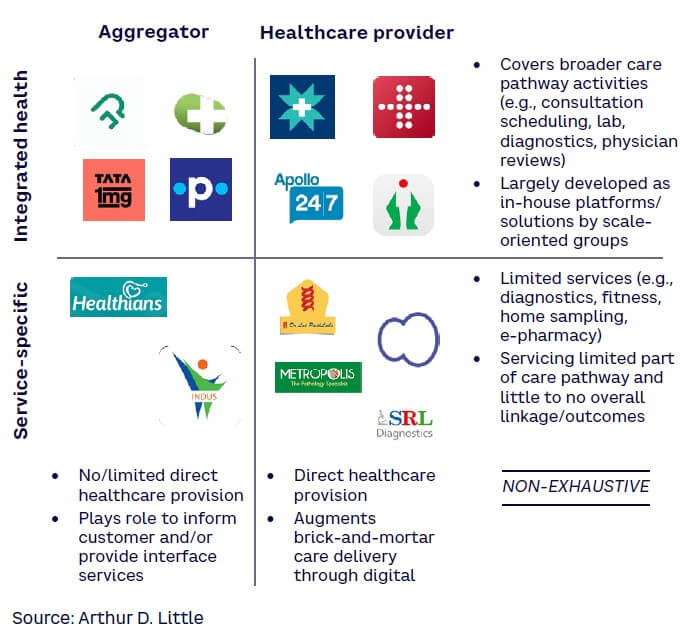
From an operations standpoint, a variety of digital offerings have been deployed by healthcare providers in the country. These span information management applications such as health information system platforms, supply chain management and vendor management platforms to integrated financial and management reporting systems.
Digital health adoption & acceptance among Indian consumers
To understand the core drivers underpinning the digital health consumer in India, ADL commissioned a broad-based consumer survey administered across the country. Longitudinal data collected from prior surveys and focus group discussions were also used to draw upon and understand recent trends and validate findings. Several key trends have been observed in the customer survey that bring to light the behavioral trends observed among digital health consumers in India:
- Deep penetration of digital health solutions, with significant room for growth. ADL’s survey indicates significant traction among consumers on the use of online pharmacies, physician consultations, and fitness and wellness applications (see Figure 3). All these applications observed between 35%-65% acceptance among customers who utilize e-commerce services. This indicates that as many as 400 million Indians already have experience utilizing healthcare services. Specifically in the case of online pharmacies, experiential similarity vis-à-vis e-shopping and online retail have helped them to deeply penetrate in the telehealth space. The survey found lower traction in e-diagnostics, which is understood to be due to perceived lower quality and accuracy of diagnoses, patient desire not to interfere with physician recommendations, and the facility operations (turnaround time, reputation, etc.). In addition, a clear divide is visible among the key age groups in the acceptance of digital health tools, with those over 40 being about a third less likely to use digital tools than younger consumers, largely because of familiarity and tool awareness among the younger population (see Figure 4). The opportunities do remain relevant for this segment, however, as increases in routine health examinations and lifestyle ailments begin to emerge among the population in the 41- to 50-year age bracket.
- Larger, more evident value pools in Tier 2 and 3 cities. Except for adoption of e-diagnostics and online pharmacies, which vary somewhat, all tiers of cities have a comparable degree of adoption for digital services, indicating that the technology divide prevalent in the past is now abating (see Figure 5). Tier 2 and 3 customers are also becoming increasingly aware of the benefits of digital technologies in healthcare and are demanding conveniences from digital health offerings.
- Stickiness is high among patients using digital healthcare services. Patients who had long-term disorders/ailments such as cardiovascular disease, diabetes, hypertension, or allied indications reported significantly higher adoption of digital health tools (see Figure 6). These patients tend to use healthcare services more regularly and in a more organized manner. As these patients adopt digital healthcare solutions and appreciate their value, they will utilize platforms even more. Digital health solutions must therefore target greater usage of digital tools and track the value of health information communicated to the consumer pool. While patients with chronic illnesses do appear to have a higher degree of adoption of digital health tools, COVID appears to have catalyzed sustained use of digital healthcare tools in India (see Figure 7). Patients were initially compelled to utilize digital channels for care needs due to movement restrictions and infection risks. However, once they experienced the benefits of digitally enabled healthcare delivery, these are now increasingly considered as necessities. It is no surprise that only ~14% of respondents accustomed to using digital health services indicated a preference to return to offline modes for health.
- Seamless integration across the consumer journey is critical for success. Key pain points for consumers remain in the brick-and-mortar components of health (see Figure 8). Many of these can potentially be resolved through digital health offerings, but only if there is a deeper integration of tech solutions with brick-and-mortar care delivery. Physical interactions — if minimized either through implementation of videoconferencing, telehealth, or remote healthcare solutions, or through application-based updating and support, or through operational transformation to ensure ready access to findings and medical supplies — can help in improved uptake and easier access to patients (see Figure 9). In addition to the above pain points, several experiential and non-transactional aspects of digital care delivery are important for customers.
- A preference for integrated applications that provide the whole spectrum of healthcare offerings. Consumers reported that applications that provide several healthcare services along with the option of storing health records are preferred (see Figure 10).
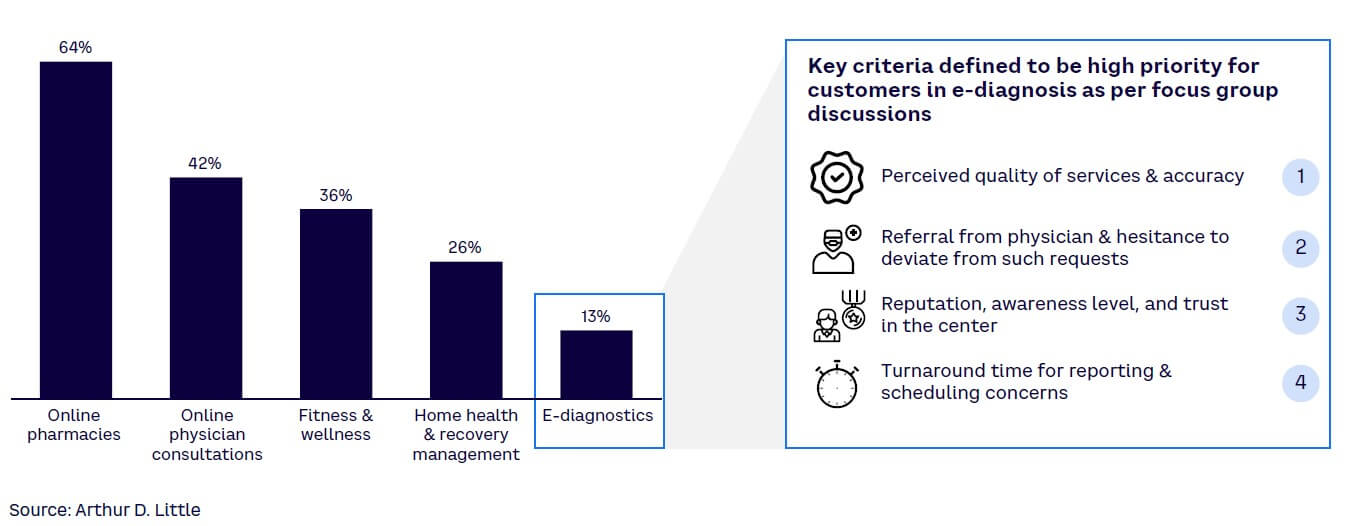
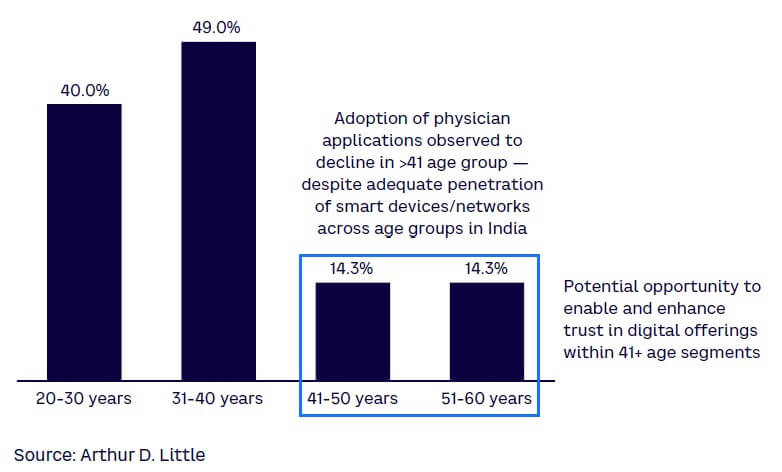
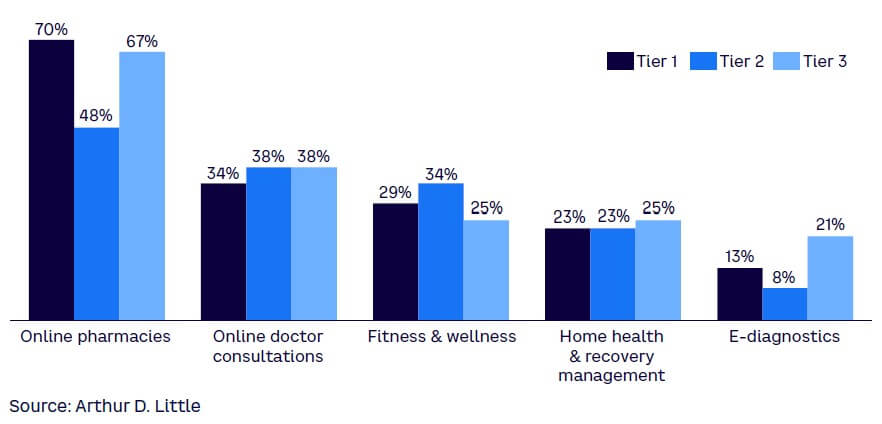
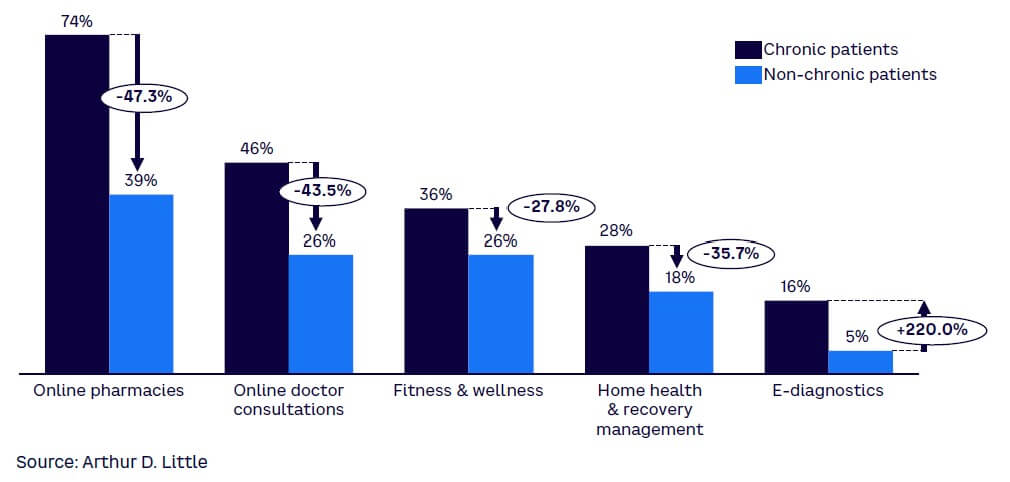
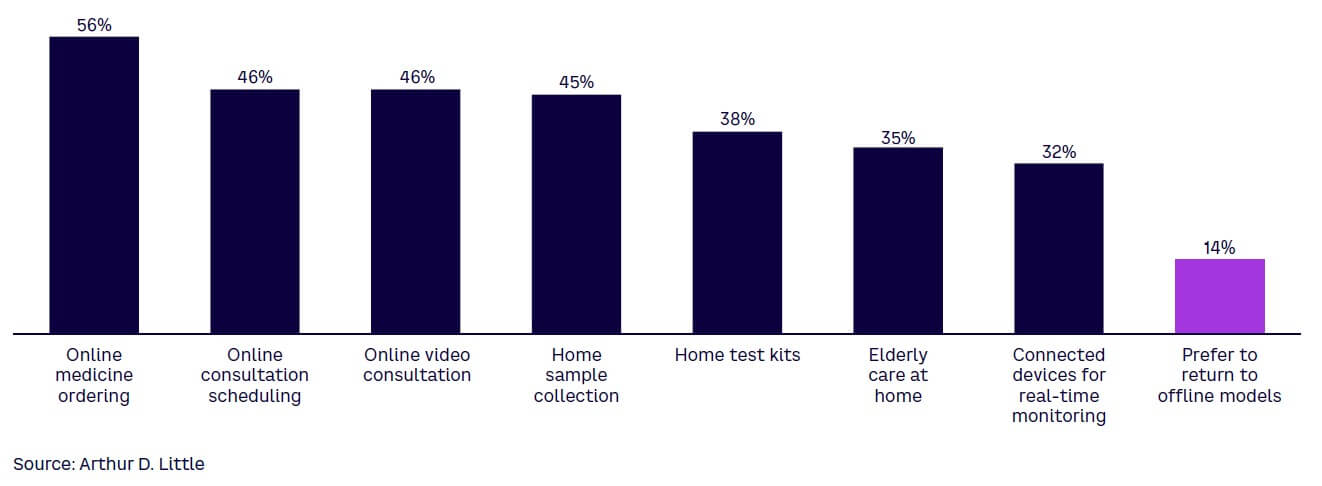
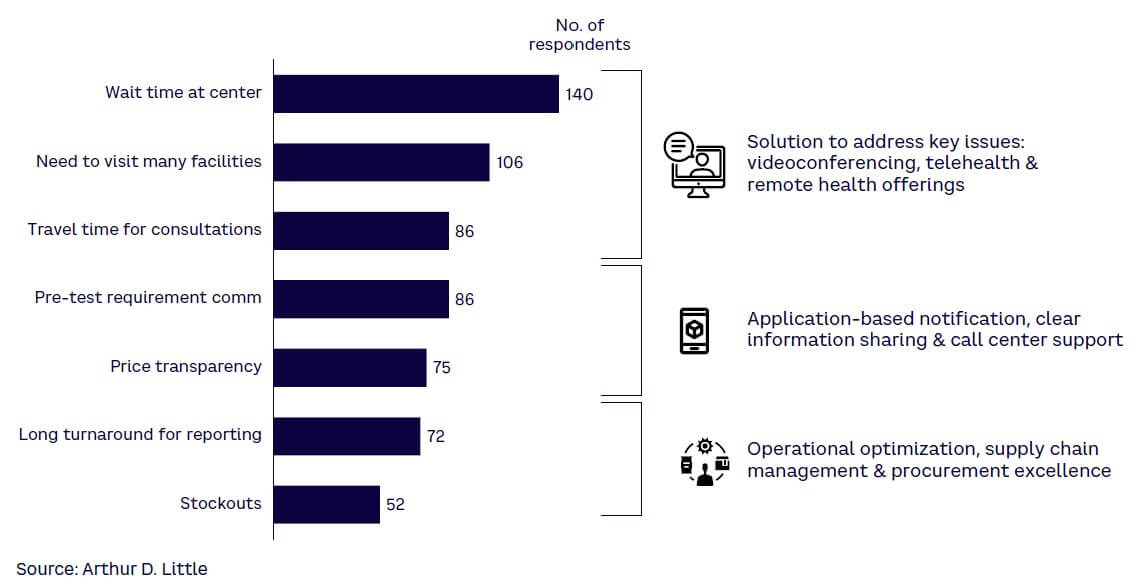
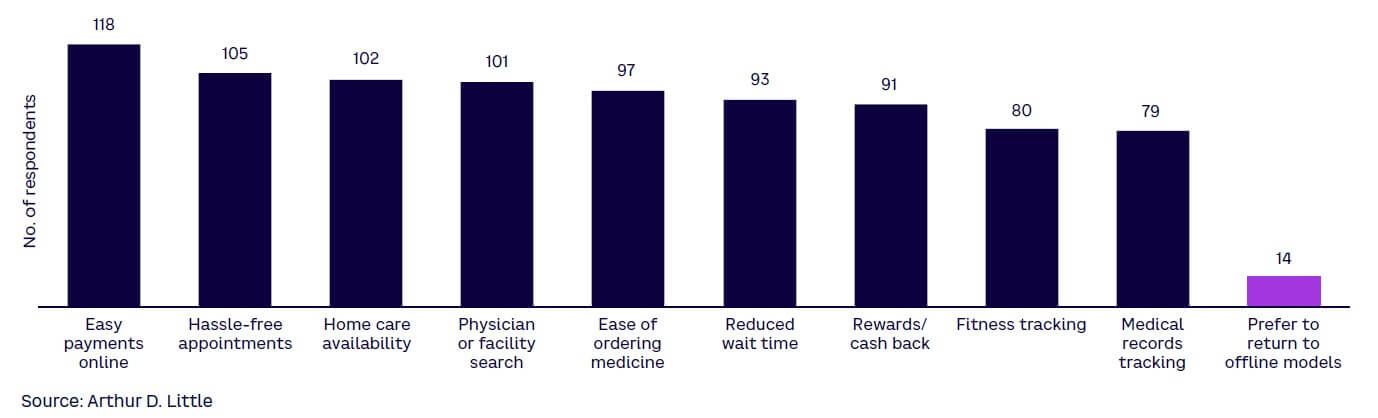
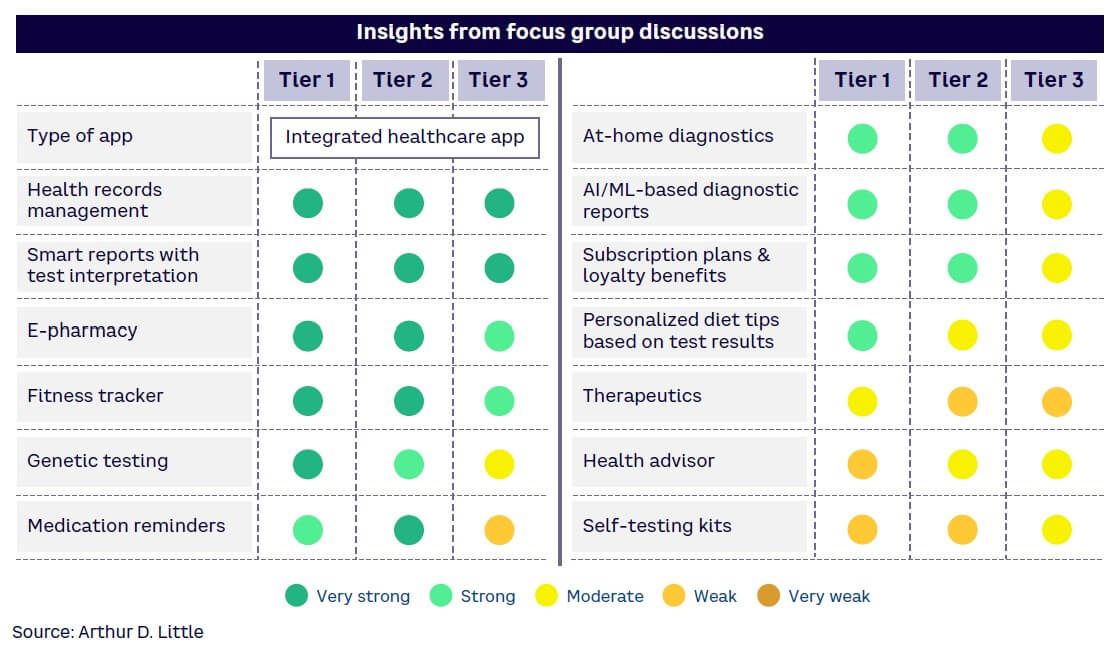
5
DIGITAL HEALTH OPPORTUNITIES IN INDIA
The case for at-scale digital adoption in India
The Indian healthcare system faces several structural and strategic challenges that create opportunities for novel and innovative healthcare solutions. India’s healthcare capacity — in terms of infrastructural capacity and caregiver coverage — remains behind regional and international benchmarks for both.
For example, in terms of bed density, or the number of beds per 1,000 people, India currently ranks lower than international benchmarks as well as most regional economies (see Figure 11). This is compounded by the fact that in Tier 2 and 3 cities and beyond, healthcare systems and access are significantly challenged and undersupplied.
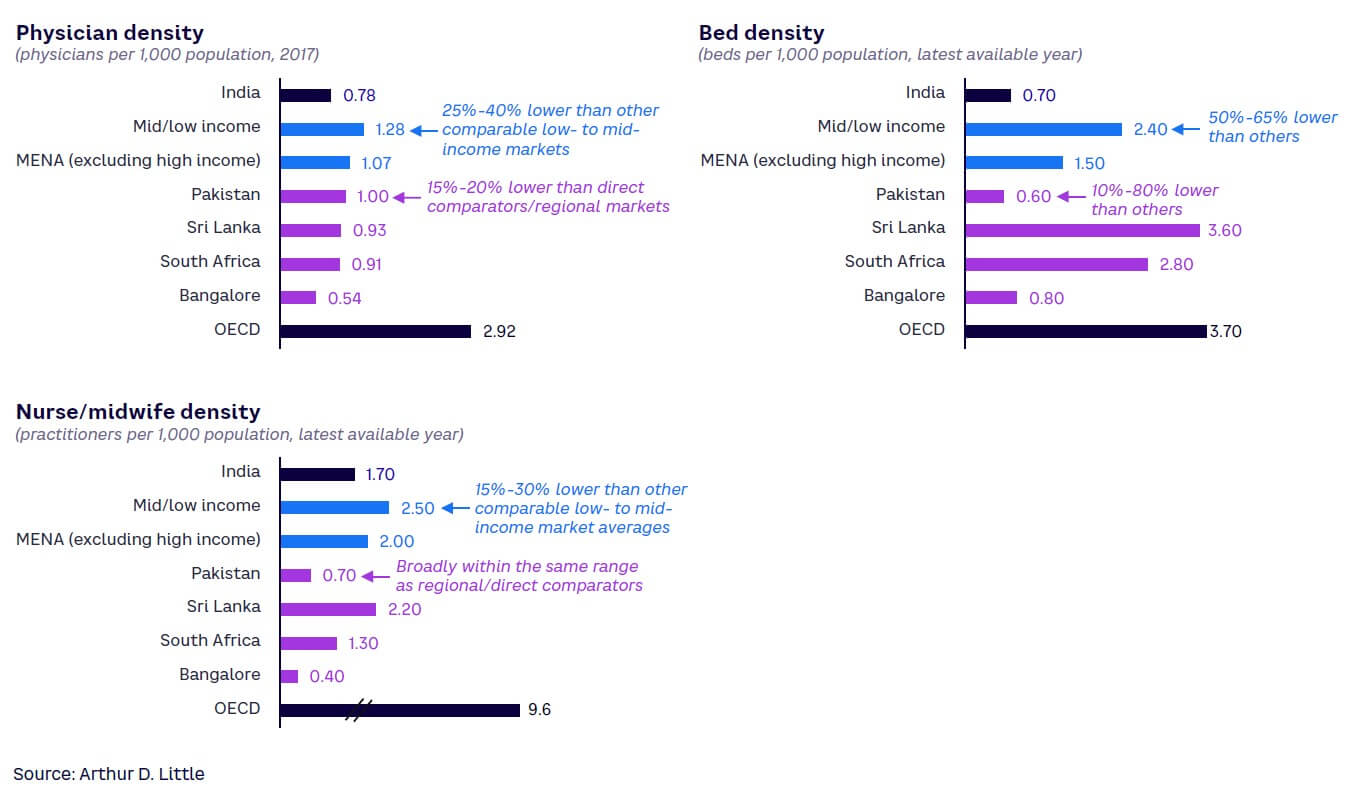
From a care delivery staff perspective as well, India is largely under-resourced to deliver care to its citizens compared to international as well as regional benchmarks. Plugging these gaps conventionally may require incrementally training and developing thousands of physicians, nurses/midwives, and other clinical staff, likely a herculean challenge given the time required to educate, train, and nurture a high-performing healthcare practitioner and the limitations that exist in health education infrastructure in the country.
At the same time, from the perspective of utility infrastructure (power and water access, etc.), telecommunications infrastructure deployment, and information access, India has made significant strides in the recent past — creating an effective foundation for digital health platforms and solutions. In fact, India now boasts the second-largest number of cell phones anywhere in the world, and smart device penetration stood at about 54% in 2020, up from only 22% in 2016.[4] With omnipresence of low-cost smart devices, penetration is expected to reach near full saturation by 2030-2035. India also had among the highest data usage globally, at about 12 GB per month per user in 2020, a number that is expected to double by 2025.[5] As 5G network access becomes accessible to urban centers, the digital revolution in healthcare will have an effective connectivity backbone.
Potential impact of ABDM deployment
In addition to infrastructure and connectivity-related interventions that have progressed rapidly in recent years, healthcare policy in India has also been aimed at creating a foundation for digital healthcare innovation through the Ayushman Bharat Digital Mission (ABDM) program. ABDM primarily aims to improve the quality and knowledge base of India’s healthcare sector in a consistent, unified, and standardized manner.
The ABDM program is critically important to affect a step change in digital health platforms. With a primary objective to establish a health data capture framework, the program can support the eventual development of a “single source of truth” for personal- and facility-level health data across the entire population of India.
The core of the ABDM program is the Unified Health Interface (UHI) framework. Reliable sources of data and leveraging that data to analyze performance and drive improvement are critical to supporting and sustaining an eventual insurance-covered healthcare model.
As information travels across the continuum of care, it becomes difficult to measure healthcare quality and facility performance. The UHI is targeted at providing a consistent data foundation that delivers actionable information to all health stakeholders and policy makers from a consolidation of various data sources. The UHI is envisioned to:
- Streamline the digital health service experience for providers and patients by establishing and standardizing the technology pathways that enable such services to be given.
- Provide an open protocol for various digital health services, including a UHI Network, an open network of end-user applications (EUAs) and participating health service provider (HSP) applications.
- Enable interoperable connections over a nationwide decentralized, open, secure, and inclusive network, using ABDM registries that keep a list of the entities participating in the network and utilize gateways that enable communication using standard protocols.
Ensuring safe storage and easy access of medical records and access to accurate information on healthcare providers will allow better decision making by the Indian government. Geography- and demography-based monitoring and effective evaluation of various programs and interventions will enable the government to adjust depending on patient outcomes.
The overall architecture of the program includes a four-layered structure:
- A unique identification database that includes public digital goods such as the Aadhaar unique identification number for patients, facility registry for hospitals, and professionals registry for practitioners.
- The collection and maintenance of health data at the patient, practitioner, and facility levels.
- A unified health interface to enable consistent and secure access to relevant health information.
- User applications such as the COVID-19 tracker Aarogya Setu and other cases to deploy solutions that accept information from the UHI layer.
The program, upon full implementation, has the potential to realize several benefits to stakeholders across the healthcare ecosystem. For key participants, there may be several opportunities:
- Patients — a singular and consistent clinical history will enable better diagnosis and comorbidity management, easier case reviews and second opinions, better availability of health data resulting in diversified and lower health premiums, reduced transaction time and costs for health insurance, and systematic tracking of health progress.
- Healthcare professionals — collecting standardized and unified health information will enable better clinical decision making, greater data availability for patient treatment, better and easier assessment of clinical risks, and easier and more streamlined clinical protocol monitoring.
- Healthcare providers — enabling community partnerships, easier linkage with governmental and social programs as they get deployed, greater access to patient pools, better clinical risk monitoring, better morbidity management/tracking, and enhancing competitiveness vis-à-vis other market participants. Effective data use can also enable catchment expansion for high-quality and efficient facilities as well as reduced marketing and patient outreach costs, resulting in increased visibility of the hospitals’ doctors.
- Health insurers — optimizing the insurance lifecycle, as adopting the health ID as a patient ID could enable consent-based access to linked health records. Opportunities exist as well in policy portability and information exchange, allowing patients to link a single health ID to multiple provider and insurance IDs for cross-insurer consistency checks and fraud prevention. Policy premiums may also be optimized for lower-risk/healthier individuals, and more diversified and larger risk pools may be enabled.
- Researchers — enabling clinical variations for enhancement in care pathways, new product development, clinical trials management and selection, and outcomes enhancement.
- Policy makers — effective capacity tracking and monitoring, surge capacity management, and redirection of policy initiatives toward emerging areas of lacunae.
Opportunities for digital health across care continuum
The opportunities that arise with ABDM have the potential to make healthcare delivery in India much easier and faster by leveraging information and communication technology. Given the market gaps and digital access enablement for external solutions, coverage and capability improvement measures may represent significant growth opportunities in the Indian marketplace. Use cases that likely will gain traction in the market center around:
- Digitally enabled home healthcare, chronic care, and extended care. Home healthcare for chronic diseases and lifestyle ailments may offer potential for digital enhancement. Patients and families of patients have historically relied on fragmented and unstructured recruitment of home healthcare practitioners through personal networks, regional ads, and so on. Aging and life expectancy increases have resulted in a rise in clinical care being provided in a home setting. These services potentially can be aggregated and provided in a bundled format at home.
Several use cases emerge in geriatric care and home healthcare involving the use of IoT and wearable devices. For example, GPS devices that track and monitor patients may be affixed to a patient’s clothing or person to assist caretakers in cases of patients with cognition challenges. Geofencing can also be used to alert caregivers to patients who leave or cross certain thresholds or boundaries. Tracking patients on an active basis allows patients freedom in movement within and outside facilities while retaining the ability for caregivers to find and assist in case of an emergency.
Wireless home-monitoring technology solutions are also becoming increasingly mainstream as streaming video devices become more miniaturized, energy efficient, and better networked even in markets with lower disposable incomes such as in India. These technologies allow caregivers to identify and monitor patient behavior and in-home appliance usage to minimize risks associated with injuries, enabling greater household safety and speedier response in case of adverse events.
- Preventative care enabled through IoT devices. Wearable sensor technology to track routine activities such as walking patterns, location and positioning, fall/injury detection, emergency messaging/SOS, and heart rate or vitals monitoring also enables caregivers to provide and extend care to larger patient pools while also providing more customized care and monitoring of specific cases. IoT devices are becoming increasingly affordable — particularly wearables — and are gaining traction among the population, with wearables alone registering growth of 93.8% by volume, according to India Brand Equity Foundation (IBEF). Large market shares are being captured by value segment players like Noise, boAt, Realme, and other players launching products in the affordable INR 3,500-6,000 range. Collected data from sensors over a period — if collected in a platform approach — can be used for preventative care rather than responsive care as well.
- Electronic medical record (EMR) adoption and diagnostic data integration. EMR adoption is the next digital frontier in Indian healthcare, primarily driven by the ABDM. The next wave of growth in medical data generated from health information systems is catalyzing the next iteration of care delivery — utilizing big data and evidence-based care and applying these principles to enable:
- Precision medicine — utilizing research and centralized data to promote enhanced diagnostics and personalized patient care.
- Safety practices — use of predictive analytics to promote quality care and patient safety (e.g., infection risk monitoring).
- Population health management — utilizing analytics in epidemiology (e.g., linking EMRs with GIS to identify healthcare trends in specific areas).
- Readmission analytics — analyzing EMRs to reveal trends that highlight patients likely to need additional treatment to prevent readmission.
- Data security — securing medical records by identifying changes in network traffic or behavior that indicates a cyberattack.
- Insurance claims — improving the efficiency of medical insurance claims by revealing claim trends and streamlining claims processing.
- Consistency and standardization in data being collected from diagnostics can also allow longitudinal tracking of key biomarkers.
- Tech-enabled capacity augmentation. Concepts such as e-ICUs and virtual hospitals (some of which are already under pilot deployment with start-ups/large healthcare groups) enable efficient deployment of critically scarce intensivists while also enabling asset-light operations in the conventional healthcare delivery approach. e-ICUs and virtual hospitals may allow several advantages over conventional facilities, including lower headcounts (on a per patient served basis) for highly trained and skilled intensivists, reduced risk of nosocomial infections due to lower contact, reduced hard CAPEX cost in real estate components of healthcare provisioning, and superior distribution of super-specialty intensivists’ capabilities across a wider group of healthcare facilities or geographical centers.[6] Consultations in India represent another digital opportunity — both for primary care visits as well as post-care follow-up discussions. India is also a significant healthcare destination from a Medical Value Travel (MVT, meaning travel in pursuit of healthcare) perspective. Historically, India’s positioning as an MVT destination has been largely on account of the high quality and deep experience of physicians practicing in the marketplace, significantly cheaper cost of care on a dollar-to-rupee basis, and the soft-power presence of India as a nation, with the capacity to advance foreign policy objectives and priorities through noncoercive means. Opportunities exist for digital health to provide pre- and post-procedure support through digital offerings.
- Scalable supply chain and aggregated value-based procurement solutions. Healthcare provider networks in India straddle a large spectrum of capability areas and sizes — from single-facility family-owned healthcare organizations to integrated and broad-based chains with dozens of hospitals operating thousands of beds across multiple cities. Smaller players represent opportunities to aggregate supply chain services under a data- and digitally enabled umbrella.
- Predictive/prescriptive digital supply chain management solutions. For large-scale players, standardization is a critical factor enabled by digital offerings. Processes, such as procurement of any materials, their management, and tracking, need to be made consistent across network/s. A universal approach leads to effective supply chain and vendor management as systems move to a central procurement management model across the entire spectrum of supplies. A digital health use case that may be deployed at scale is predicting the nature and amount of stock moving at a certain point of time, based on historical demand/supply data. Automating procurement functions and configuring reorder levels, inventory levels, reserves, and stock-out levels can all be optimized through effective use of digital offerings. Value-based procurement can be enabled through use of analytics and big data. Such systems, if executed well, can also provide necessary checks from a supply chain governance perspective. In addition, systematic tracking to prevent pilferage and misuse of items can lead to significant revenue losses. Systems should also be integrated in the financial systems, such as invoicing and digital payments. Integration and automation of supplier reviews and consolidation of supply also supports the maintenance of relationships with vendors and suppliers.
- AR/VR-based training in specialized care. AR/VR-based applications represent opportunities for a variety of training and capability development sessions. For low-complexity physician education programs by pharma and medical devices companies, pure AR/VR solutions may suffice. However, for more technically complex medical devices/implant-based training and development activities, mixed-reality applications are also emerging — reducing the training gap by enabling physicians and care givers to gain tactile experience in addition to audiovisual experiences.
- Digitally enabled aggregation for standalone facilities. A large majority of India’s healthcare system is disaggregated and consists of standalone facilities. These facilities may not have the scale to reap benefits from digital health enhancements even if they choose to invest. Capabilities to effectively deploy effective and integrated digital health solutions in these facilities may also be a constraint in a large majority of such facilities. Nor will it be easy for smaller facilities to comply with or leverage the unified health information structures that will be rolled out under the ABDM program. This represents a clear opportunity for health tech enterprises to develop modular, scalable, customizable, and easily implementable solutions for such players. Similar opportunities also exist in digitally enabled supply chains and procurement value creation initiatives. Standalone facilities may have demand variabilities and challenges in integrating digitally with suppliers. These facilities may not have the right capability set to push value-based procurements concepts viably. However, intermediaries who can aggregate and can digitally interface with both suppliers and consumers can potentially facilitate the process, offering predictability, managing economic order quantities, and enabling efficiencies in procurement.
- Medium- to long-term opportunities. In addition, several other opportunities can be digitally enabled and made more effective. For example, digital loans, with funding linked to clearly defined digital readiness and easier financing access, can allow health organizations to invest in digital and improve their “digital internal rate of return.” However, this may require the digital health ecosystem in India to become more formalized and for digital health players to become more standardized and segregated. As digital penetration starts to hit critical mass, the middle- and lower-income segments in India will also start to become viable from a service-delivery perspective. These segments already have growing penetration of smart devices and platforms to support digital health. With increasing availability and critical mass, the fortune at the bottom of the healthcare pyramid in India can become digitally accessible as well.
Over the longer term, as the overall health delivery system matures, India may move toward coordinated health, and eventually toward a managed health network. However, this will require the entire ecosystem to be able to exchange information on a common framework — something that will be enabled through digital health offerings.
CONCLUSION
11 IMPERATIVES FOR INDIAN HEALTHCARE ECOSYSTEM
India presents a unique opportunity for an existing digital health user community of 400 million people. With the further penetration of smartphones, 5G adoption, and service provider innovation, by 2030 India could easily have over 1 billion digital health users. This will help catalyze a transformation in Indian healthcare, creating the platform to provide quality, affordable care to all Indians. The government has also created a scalable technology architecture (through the ABDM) for healthcare ecosystem players to drive technology-led transformation of the sector. The healthcare industry now needs to step up and break through the digital divide. To realize the full potential of digital health, we propose the following imperatives for the various industry stakeholders.
Provider imperatives
Providers remain the foremost point of interaction between end users and health systems. While COVID has accelerated the digital uptake and improved accessibility, a lot of providers look at digital to be another business unit rather than a force multiplier. Providers must ensure integration of digital systems within the provider space and other stakeholders to enable meaningful digital changes and use of digital first as a strategic advantage:
- Digital first. Providers face a risk of getting disrupted by digital interventions, entrepreneurs, and competitors unless they have a digital-first strategic outlook. It is essential that they create deeply integrated offerings to capture and retain the consumer base over the long term. At the same time, digital should not just be considered as a front-end/patient interface activity and should be cost effective and focused to capture efficiency gains. At the same time, emphasis should be on building digitally enabled supply chains that are resilient, scalable, and efficient.
- Platform offerings. Healthcare offerings have specialized and moved beyond the confines of hospitals. A variety of services and products are home-based, hospice-based, or can be used anytime/anywhere. To improve customer loyalty and stickiness, it is essential that product and service availability be improved through a platform approach. This would require providers to partner with each other, payers, and other stakeholders to create meaningful health service platforms.
- Partnership strategy. The rising complexity and scale-up challenges of digital product development make it imperative that providers do not build everything and instead try to reduce the risk of failure. Build-buy-develop decisions and consequent actions are vital. A provider must have a strategic need-solution analysis framework and an ecosystem that helps them to integrate multiple products easily. This must also be reflected in operations, strategy, human resources, and advisory capabilities.
- Data strategy. With the advent of digital capabilities, providers are required to collect, manage, and store large amounts of data. This data can provide intelligence to personalize offerings and improve customer stickiness, but it requires a detailed digital data strategy to ensure the organization uses the data within the confines of regulations and privacy. Providers may develop the data strategy along with offerings to comply with regulations while utilizing the multiple benefits of healthcare data.
Payor imperatives
Healthcare payers have traditionally dealt with a fragmented ecosystem, which has resulted in multiple redundant systems to distribute products, process claims, and reduce fraud. Digital products can solve these redundancies by reducing the cost of acquisition and improving the efficiency and effectiveness of claims processing. The ecosystem needs products that can solve for both the payor and end customer while ensuring seamless integration with provider systems:
- Digital insurance distribution. The penetration of insurance products in India is poor, and few start-ups and digital disruptors have taken up the opportunity to digitize distribution, posing serious challenges to existing players. Payors must identify the opportunity, develop digital distribution platforms, and partner with providers and other stakeholders to enable digital transformation in their business. This would entail developing a strategic vision in developing the offering while ensuring customer focus and ease.
- Health claims platforms. Rising healthcare complexity — with instances of fraud, misrepresentation, and increases in volume — exposes payors to financial and operational risks. This can be mitigated by integrated health claims platforms with claim, disbursal, fraud detection, and analytics with minimum human effort and cost. Providers must have a strategy toward development and deployment of the claim platform and integration with providers, distribution, and regulators to ensure low risk and higher efficiency.
Regulatory imperatives
While regulators and policy makers have taken steps in the right direction, they will also need to become the system’s conscience as digital offerings are rolled out. The most critical imperative for policy makers will be to ensure the program is governed effectively and appropriately. Data access, availability, and privacy are concerns of global consequence and, with greater consumer awareness, it will be necessary for regulators to be the custodians of the health data that is generated:
- Regulatory framework. Being an ombudsman looking to balance compliance with the prescribed standards and commercial and policy support considerations.
- Start-ups. Supporting new and incumbent digital players to garner and secure funding for health tech start-ups.
Investor imperatives
Investors remain the key accelerating force in every industry, and that is no different in digital uptake in healthcare. Investors have always welcomed digital offerings and solutions to improve efficiency and margins. However, investors must undertake systemic changes to ensure digital products in healthcare are integrated, drive enhancements in the health system, and reach the end users for whom they have been designed. These changes include:
- Targeted digital financing. As the start-up ecosystem and linked investor base start to deploy resources aggressively in new product and service line development and new ventures targeting digital health opportunities, an attractive and independent ecosystem could gradually emerge supporting digital-first offerings. These will need to be nurtured and effectively managed by the investor group while ensuring digital ability is considered as integral in deal flow and screening processes, and not just an incremental differentiator. In parallel, the start-up ecosystem must integrate and penetrate brick-and-mortar healthcare delivery to enable access to care.
- Driving true integration. A digital-first investment/resource allocation approach should not become a “digital only” approach for investors and health tech start-ups. True integration is only possible with both the digital and brick-and-mortar realms being seamlessly integrated. Ensuring investment/M&A targets will need to be screened and scored with a quantitative approach. All of these should be targeted at developing an attractive, independent, and lucrative investment ecosystem for investment in health, health tech, or digital health trends. Digital health should also be considered by investment houses during the deal evaluation, deal assessment, and, eventually, a value creation plan.
- Novel financing areas. Investors need to finance digital health innovations and platforms through greater emphasis on health tech and insurtech start-up ecosystems. This would enable growth of the entire ecosystem and add value to innovators and disruptors.
India stands at the cusp of a revolution in healthcare access, with several public healthcare schemes as well as increased private interest in healthcare delivery. Digital remains the most potent force multiplier to enable a mature and efficient health system. These 11 imperatives are key to unlocking value while moving to a digital-first healthcare system and ensuring that the system is integrated, efficient, and has participation from all stakeholders.
Notes
[1] “Noncommunicable Diseases.” World Health Organization, 16 September 2022.
[2] “2022 World Population by Country.” World Population Review, accessed October 2022.
[3] “Medical Devices Market — Growth, Trends, COVID-19 Impact, and Forecast (2022-2027).” Mordor Intelligence, August 2022.
[4] “Smartphone Penetration Rate in India from 2010 to 2020, with Estimates Until 2040.” Statista, accessed October 2022.
[5] “Average Data Consumption per User per Month in India from 2015 to 2021.” Statista, accessed October 2022.
[6] Iyengar, Karthikeyan P., et al. “Electronic Intensive Care Unit: A Perspective Amid the COVID-19 Era — Need of the Day!” Lung India: Official Organ of Indian Chest Society, Vol. 38, Supplement, 2021.
DOWNLOAD THE FULL REPORT