16 min read • Healthcare & life sciences, Information management
Hospital Information Systems for the digitally-enabled era
A new wave of innovation within healthcare is driving the need for more advanced, robust and scalable hospital information systems


Executive Summary
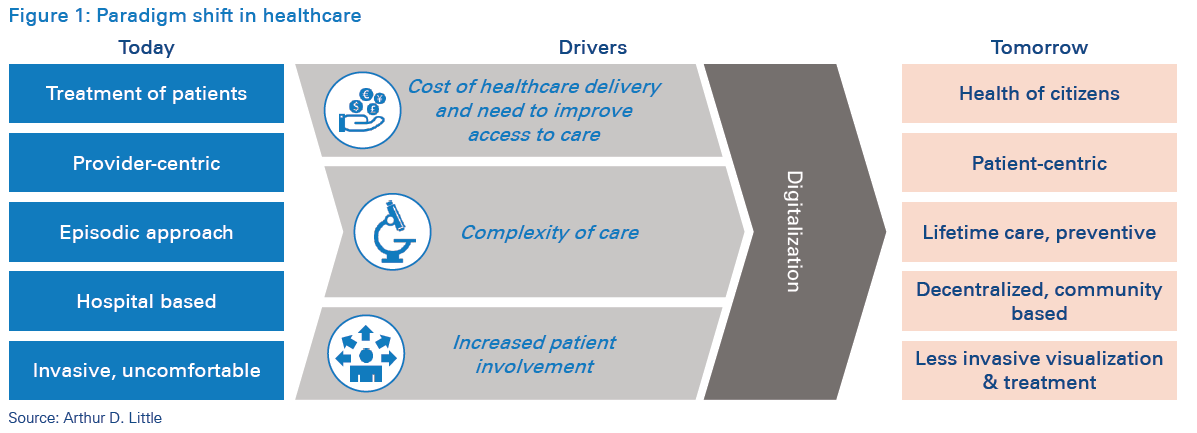
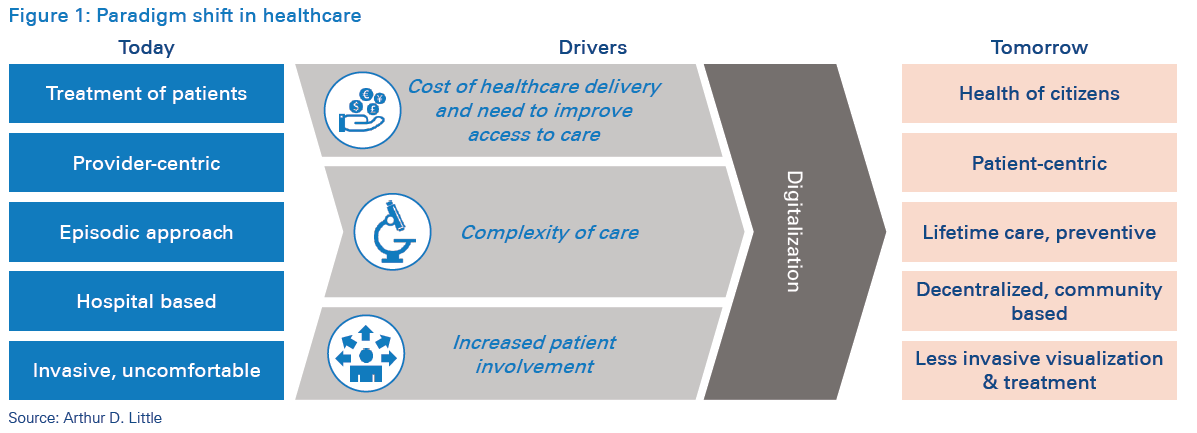
Healthcare is undergoing a paradigm shift driven by several factors. New models of care are emerging, focus is shifting from illness to wellness, and costs continue to climb amid rising demand for personalized, long-term care and the need for patients to participate in care management. Increasing expenditure on global healthcare delivery is unsustainable, which is making innovation and transformation imperative for sustainability. In this Viewpoint, Arthur D. Little analyzes how healthcare providers are starting to reorient their investments in hospital information systems’ other core technologies, and how technology vendors are adapting their solutions and services to meet these needs.
1
A new paradigm in healthcare delivery
The healthcare industry is undergoing radical change and disruption globally. New and emerging technologies such as artificial intelligence, powered analytics and diagnosis support, edge and secure cloud computing infrastructure, the internet of everything, and blockchain information exchange and interaction enablers, as well as practical technologies such as 3D printing and robotic surgery, are all changing how, where, and when healthcare can be delivered.
These developments combine to enable a fundamental shift towards coherently integrated health systems, in which multiple stakeholders (providers, patients, insurers, researchers and regulators) interact in a continuum, with a combined focus on enhancing both the care delivery methods and the outcomes being achieved. These shifts in healthcare delivery are characterized by some key features:
Emergence of “population health management”: Patients are no longer just treated as individual cases. With digital information exchanges, health data is being aggregated at community, national and regional levels. All stakeholders in the health ecosystem are creating mechanisms to access and share essential health-related information from disparate sources, allowing detection of key medical trends with greater speed and accuracy.
Patient centricity: Delivery of care is being tailored towards specific needs, preferences and patient values through increased digitized engagement models. Providers are focused on building personalized treatments, which create positive impact on outcomes and the overall patient experience.
Preventive- and lifetime-care approach: Advancements in medical knowledge and abundance of information dissemination methods are increasing patient awareness and participation in the management of their own wellness. Providers and regulators alike are focused on increasing people’s knowledge of medical conditions, symptoms and care options to encourage them to take a more proactive approach towards health management. Moreover, medical scientific advancements are going to make curative treatments available to patients with severe conditions.
Decentralized care: Patients now have access to high-quality care well beyond the confines of traditional geographical boundaries. Increasing use of telemedicine is creating a decentralized model of operation among health facilities. Increased availability and adoption of technologies in home care are extending care interaction well beyond the confines of the traditional hospital. This is transforming the traditional hospitalbased care-delivery model into an integrated but dispersed model of care management.
Non-invasive treatments: Advancements in medical technologies are creating a new generation of minimally invasive treatment options, thereby reducing dependence on complex physical infrastructure needs and reducing the duration of care delivery. Such treatment options, coupled with those to deliver such care outside the confines of the traditional hospital setting, are fundamentally altering how patients will experience health services in the future hospitals utilizing hospital information systems traditionally included 14 core modules to run their operations.
2
Factors driving the paradigm shift
A number of factors have contributed to this rapid shift in the health management and care delivery paradigm – rising costs of service delivery, the need to improve access to care, greater patient involvement in health management, and underlying technological advancements to improve outcomes. Moreover, health-service providers are facing challenges with health information exchange. Sharing health information can help health providers reduce readmissions, avoid medication errors, and even decrease duplicate testing. However, there are continued concerns about how to efficiently and effectively access data/ information for health professionals to conduct their jobs efficiently and safely. This also holds for other stakeholders, such as pharmaceutical companies and research institutions. In addition, there are growing concerns regarding how to keep data secure, ensure interoperability of various systems, remain competitive (e.g., sharing data among competitor health-service providers), and successfully implement the transformation program for the paradigm shift towards a digitally enabled era.
These factors have been strengthening with a shift in global demographics and increased demand for health services. Dramatic changes in lifestyle and increased average life spans that exponentially raise the demand for health services are making the underlying imbalances escalate.
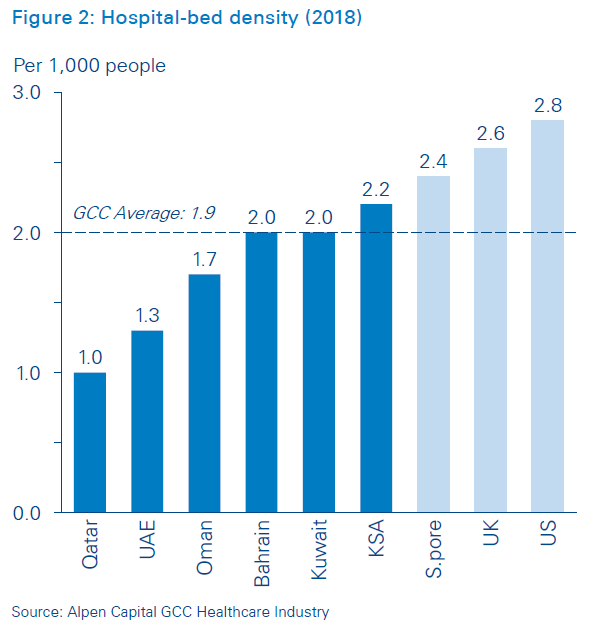
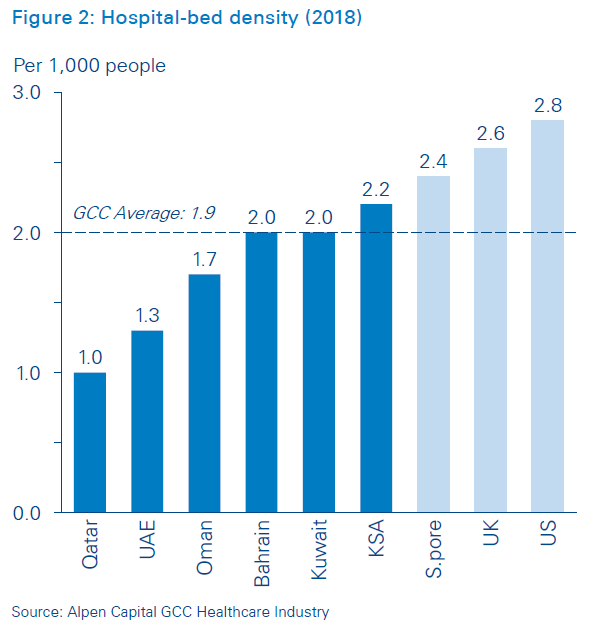
We use the Middle East as an illustration. Its health systems are undergoing a significant transformation in the GCC (the Gulf Countries Cooperation, comprising the United Arab Emirates, Saudi Arabia, Oman, Kuwait, Bahrain and Qatar), which has experienced a growth in population, a shift towards an older age-group distribution, and high occurrence of lifestyle-related diseases. Local population growth bolstered by a large inflow of expats is expected to drive the GCC population count to 59.2 million by 2020 at a CAGR of 2.4 percent. Improved life expectancy has also led to a shift in the age-group distribution in which, by 2020, 15.3 percent of the population will be above the age of 50. The occurrence of lifestyle-related diseases such as diabetes, asthma and obesity have further augmented the need for healthcare services and facilities. Moreover, the high hospital-bed density in the GCC requires rethinking the way healthcare is delivered.
These changes – in addition to economic downturns and tight governmental budgets – have forced many health organizations (particularly hospitals) to change the way they deliver healthcare, as well as their operating and business models, and made it imperative to shift to a digitized healthcare system. In the midst of this digital transformation wave, the last decade has seen hospitals shifting their care-delivery models. Furthermore, with increasing maturity in technology adoption, most executives involved in the healthcare sector are increasingly focused on developing a new generation of smarter, digitally enabled hospitals, fundamentally rethinking hospital capabilities, and adopting an integrated approach to design, management and operations of their care delivery infrastructure.
3
The role of hospital information systems in the healthcare paradigm shift and challenges to driving digitization

Hospitals utilizing hospital information systems traditionally included 14 core modules to run their operations.
Hospital information systems play a vital role in digitization of care providers. Their benefits include, but are not limited to 1) improved information access, 2) increased healthcare professional productivity, 3) more efficient and accurate coding and billing, 4) higher-quality healthcare, 5) better clinical management (diagnosis and treatment), 6) reduced expenses associated with paper medical records, 7) fewer medical errors, 8) greater patient safety, 9) improved patient outcomes and 10) increased patient satisfaction.
Despite the prevalent benefits of digitization in the healthcare sector, many hospitals face difficulties in implementing new technologies in their existing service landscapes. Compared to other sectors, healthcare has traditionally been slower in adopting digitization. Three key challenges underpin the slow move towards adoption of digitalized solutions:
Technology: Integration of multiple IT systems, finding qualified and cost-effective service providers, and legacy issues.
Operations: Cultural change, particularly with senior doctors, staff, and the IT department.
Costs: Digitization is of investment intensive and added to the already-increasing cost service delivery.
Hence, the conceptualization and implementation of a digitalized hospital traditionally has been more complex than it appears on the surface. The first step towards implementing digitization in health organizations is to modernize and digitize their information systems for collecting, sharing, and analyzing large volumes of complex (and confidential) patient and other clinical information. Our vast amount of work in the Middle East and abroad supporting health organizations in innovating visions and strategies for digitalized hospitals has shown that most of these institutions find it difficult to understand and implement hospital information systems. However, this is more accurate in the Middle East than in Europe and the US. Many institutions in the Middle East lag behind in implementing these core technology capabilities. For example, adoption of electronic medical records (EMRs) in the Middle East is still trailing behind that of the US and Western Europe. This is mostly due to regulatory factors still taking shape, pushing providers towards increased EMR adoption and utilization. In the US, the 2009 HITECH Act was designed to bring hospitals into the modern era of technology and give them and physicians a reason to start using electronic records instead of paper. An incentive and penalty system was created as well.
To facilitate the adoption of these technologies, most GCC governments have laid out long-term strategic plans to upgrade their information systems. In KSA, for example, the “Comprehensive Health Program & National e-Health Strategy” has outlined 70+ projects focused on increasing HIS adoption among hospitals and PHCs, enhancing data centers and telecommunications equipment and enforcing stricter e-health standards and policies. However, hospitals still face many challenges in understanding, implementing and modernizing their hospital information systems. As most health systems shift towards adoption of these technologies, there needs to be cognizance of the rapid shift of these fundamental technologies. We have identified eight key trends that will fundamentally alter the health information system landscape. Senior executives and decision makers who are driving investments in hospital information systems need to make sure their ongoing investments cater to these emerging demands to future-proof these investments, since the pace of these advancements are significantly higher than the speed of implementation in most healthcare institutions.
4
Eight trends changing the HIS solution space
Upcoming trends in digital-health technologies, when integrated with hospital information systems, extend the boundaries of healthcare well outside the hospital walls, as well as deliver qualitative, quantitative and financial benefits to both patients and healthcare providers. Eight key trends in the digitization of healthcare are radically changing the HIS solution space:
Patient engagement: Hospital information systems are utilizing digital tools to increase participation and promote positive patient behavior. Through the use of mobile applications, interactive patient portals, text messages and e-mails, patient health outcomes are enhanced. These channels supply patients with important information, such as their personal health records and specific education about their medical conditions. They also allow patients to track their care plans, book appointments, manage prescriptions, and become more involved in treatment decision making. Allscripts, for example, has launched the FollowMyHealth® portal, which provides user-friendly navigation to encourage patients to stay connected. The engagement tool is also EHR-agnostic, which gives patients a single point of access, regardless of the different EHRs utilized by various providers.

Health analytics/artificial intelligence: Unprecedented growth of medical data generated from HIS has launched the era of health analytics and artificial intelligence in the healthcare domain. Information gathered and analyzed from patient records, drug administrations, operational data, insurance billing and regulatory sources can produce benefits in several areas:
- Performance management: Understanding of hospital performance along key metrics (related to outcomes and financials) to understand their clinical, operational and financial performance by department/clinical condition/ physician so they can identify and drive performance improvement initiatives.
- Pathway management: To optimize patient pathways within the network, as well as clinical pathways within the hospital, by coordinating care across settings.
- Clinical decision support: Utilization of patients’ clinical, physiological and longitudinal data to determine optimal diagnostic and treatment decisions so they can support clinical staff and decision boards.
- Precision medicine: Utilization of research and centralized data to promote enhanced diagnosing and personalized patient care.
- Safety practices: Use of predictive analytics to promote quality care and patient safety, e.g., early warning of a sepsis infection.
- Population health management: Utilization of analytics for use in epidemiology, e.g., linking EMRs with geographic information systems to identify healthcare trends in specific areas.
- Balancing length of stay and readmissions: Analysis of EMR data reveals trends that highlight patients likely to need additional treatment to prevent readmission, as well as patients who could be discharged earlier, so length of stay can be improved.
- Data security: Securing medical records by identifying changes in network traffic or behavior that could indicate a cyberattack.
- Insurance claims: Improving the efficiency of medical insurance claims by revealing claim trends and streamlining claims processing.
- Personalized medicine: Predictive modeling with EHR data is anticipated to drive personalized medicine and improve healthcare quality with its ability to leverage huge population sample data to identify patterns and trends and apply them to individual patient cases.
Wellness: Self-care through smartphones, tablet PCs and other communication devices has been experiencing unprecedented growth as ICT penetration and general medical awareness of patients have been increasing. Wellness supports patients in self-care through user-friendly digital applications that range from diet and weight loss to asthma care management. Lantern is a mobile application that provides support for emotional wellness through daily exercises and emotional coaching. It supports emotional wellness through cognitive behavioral therapy (CBT), helping users manage their problems by changing the way they think and behave, and also connects users with professionals through messaging and calling functionality. These digital applications can be integrated into HISs and support patient recovery by providing interactive treatment plans and monitoring progress.
Biosensing wearables: Biosensing wearables allow users to continuously measure a wide variety of metrics, and recent technological breakthroughs have made them affordable and accessible to the masses. These wearables come in an assortment of designs, from wristwatches and clothing to ingestibles and smart implants. These biosensors measure and track a diverse set of metrics: movement, heart rate, sleep, temperature, glucose, etc., and provide invaluable data points to users and healthcare providers that would have previously required intrusive methods to obtain. However, the sheer volume of available sensors and applications has presented healthcare providers with the challenge of software integration. Therefore, Leading HIS vendors have tackled this issue by partnering with technology platforms such as Validic. Validic is a cloud-based digital-health platform that connects providers, pharmaceutical companies, payers, wellness companies and health systems to over 400 in-home devices, wearables and patient-healthcare applications.
Telemedicine: Hospitals are moving towards utilization of telemedicine as part of the evolution into the patient-centric model. Previously, hospitals followed a centralized approach, which led to dramatic increases in operating costs and a great deal of travel inconvenience to patients living far from major hospitals. Through the use of telemedicine, patients and healthcare providers can now interact in real time through various communication channels and transmittal and storage of medical data, as well as remote monitoring. Epic, one of the largest US-based HIS providers, has partnered with Vidyo to provide remote healthcare services through computers and smart devices. Their product allows real-time video communication between clinicians and their patients or peers, within the same workflow tools they use for charting, accessing patient records and managing care. Telemedicine allows hospitals to decrease costs by reducing extra staff and space requirements, and increasing their ability to deliver care to larger volumes of customers.
Health information exchange: Healthcare information exchange (HIE) mobilizes healthcare data across organizations within a region, community or hospital system. There are three main types of HIE:
- Directed exchange: Sending and receiving secure information electronically between care providers to support coordinated care.
- Query-based exchange: Providers finding and/or requesting information on a patient from other providers – this is often used for unplanned emergency care.
- Consumer-mediated exchange: Patients aggregating and controlling the use of their health information among providers.
InterSystems has launched HealthShare as its strategic informatics platform for HIE. It allows effective and meaningful health-information sharing, whether for payers, within a hospital or hospital network, or across an entire region. The benefits include clear and secure access to records and improved visibility of overall population health, as well as reduced costs due to automated business processing, supported coordinatedcare management and, ultimately, reduced readmissions
However, there are continued concerns regarding how data/ information will be exchanged efficiently and effectively for health professionals to conduct their jobs proficiently and safely. This also holds for other stakeholders such as pharmaceutical companies and research institutions. There are other concerns around keeping the data secure, ensuring interoperability of various systems, competition (e.g., sharing data among competing health service providers), and implementing transformation programs for the paradigm shift towards a digitally enabled era.
Homecare: Advancements in technology have allowed patients to receive the care they need at home, avoiding unnecessary hospital visits. Patients are monitored in their homes with biosensors and PDAs, and connected 24/7 through software to emergency services, hospitals, clinics and hospice agencies. In addition, prescription management, full medical-record accessibility and digital support for homecare staff are used along the patient healing journey. Cerner’s HomeWorks® and RoadNotes® software solutions help hospice agencies and clinical staff deliver personalized homecare. Digital features support full life-cycle management of patient care, ease of transition between different levels of care, and compliance with regulatory requirements.
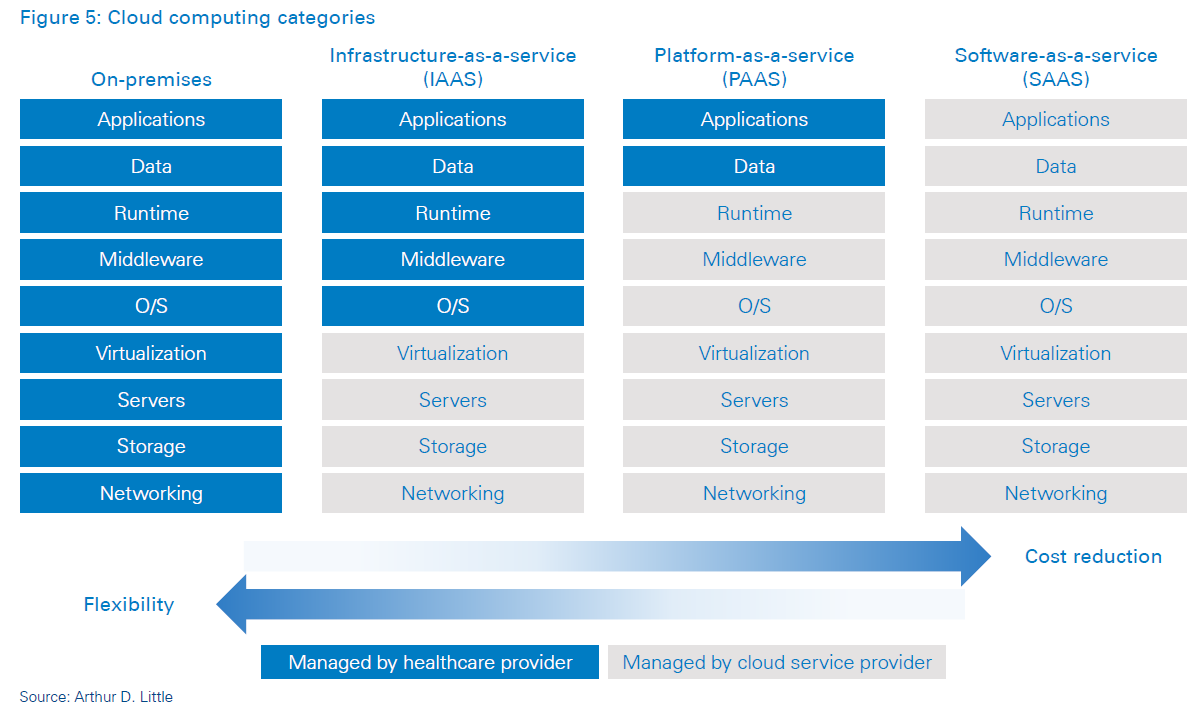
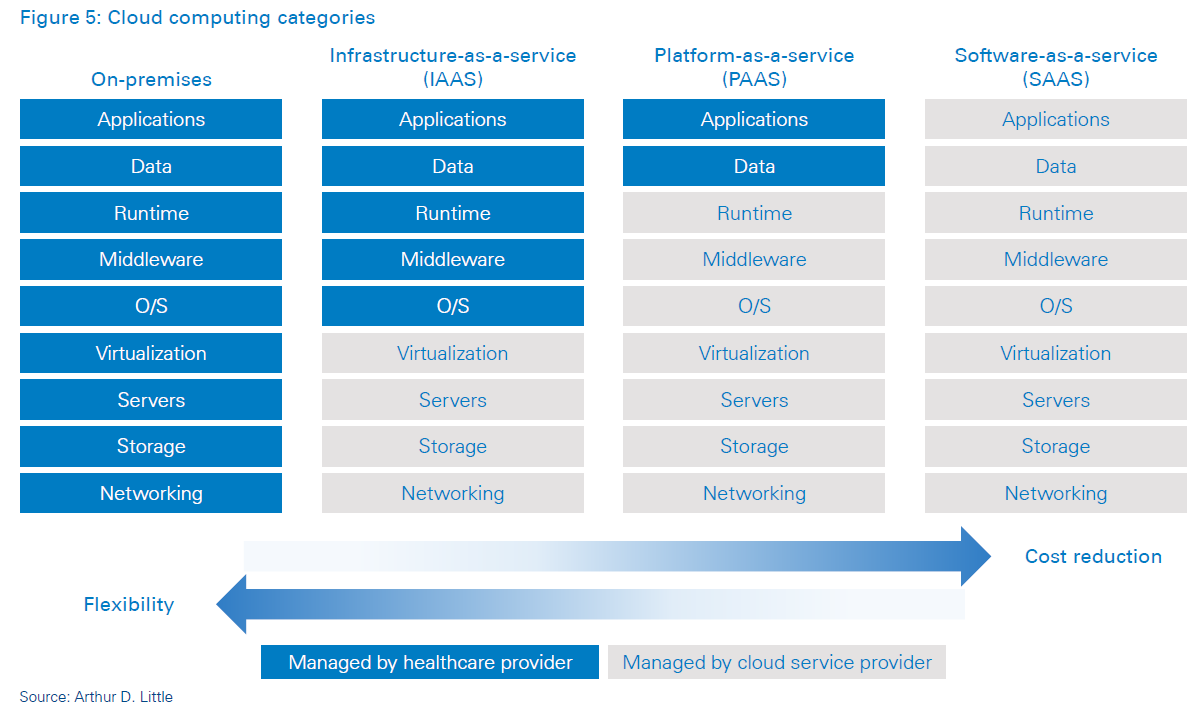
Cloud computing: Cloud computing can encourage digital healthcare adoption by reducing hospital information system startup and operational expenses. However, this comes at a cost of reduced flexibility. Practo’s Insta hospital information system is a software-as-a-service (SaaS) offering aimed at midmarket health providers. Its browser-based tools avoid lengthy and costly implementation time, and its modular product range caters to a wide variety of health providers.
There are several challenges and benefits related to cloud computing. Cloud computing does not necessarily promise lowering costs; it is more about accessibility and functionality. The main benefit of cloud computing is getting access to computing power and infrastructure that would be difficult and expensive to establish by own means, as it is not readily available in the market. The biggest challenge related to cloud computing is ensuring information security, especially when it comes to the CLOUD Act. This allows federal law enforcement to compel US-based technology companies, via warrant or subpoena, to provide requested data stored on servers, regardless of whether the data is stored inside or outside the US.
5
ADL’s view on HIS modernization
Hospitals aiming to digitize and evolve along the HC paradigm shift should aim to build hospital information systems beyond the core modules by moving towards adding more specialized modules (laundry, kitchen, anesthesia, and more), as well as connecting their existing HISs to external systems (HIE, telemedicine, biosensing wearables, etc.), depending on their needs. These updates pose challenges to healthcare providers in selecting products and vendors and implementing changes.
The first challenge that a hospital needs to address is identifying its current and future needs. Technology is ever-evolving, and a proper study of requirements is necessary to ensure selection of the right products.
The hospital should then assess which service and outsourcing models are most suitable to its operations in terms of cost and flexibility (on-premises, IAAS, PAAS, SAAS). Health providers must also look into vendor selection, adhering to single vendor options for all their systems versus going for a best-of-breed approach.
Advanced HIS platforms are heading in the direction of becoming more open in their architecture, allowing for direct integration with third-party tools and systems (for example, home-care solutions) and providing these to their patients through their websites, applications, etc. This concept will also align with the emerging patient-journey model. Hospitals could also evaluate partnering with providers such as online pharmacies, online consultation tools, and wellness management platforms, which would have a significant impact on the way they enable their service-delivery models to both patients and insurers.
Next, hospitals must address challenges that accompany implementation across the technology organization. These include: adapting system organization and workflow to suit the existing operating models or vice versa, reducing system downtime to a minimum, training staff and mitigating resistance to change, as well as ensuring data security. Addressing the challenges will require an integrated planning and design framework that includes not only technology, but also strategy, operations and infrastructure planning.
Finally, implementing HIS is not an IT project; rather, it is a large organizational transformation project requiring involvement of various stakeholders. Moreover, it is critical to involve the various stakeholders (such as health service providers) already at the outset of the HIS implementation (i.e., during the strategy development or supplier selection phase) to ensure a smooth, effective and successful HIS implementation.
Based on our experience working with hospital systems, we believe the key success factors required to achieve an effective upgrade are:
- Strong support from management and the drive to transform.
- Close alignment of the ICT system strategy with the overall objectives and vision of the hospital.
- Strong integration into clinical operations to drive new ways of working.
- Working towards a master plan with phased development rather than a scattered, piecemeal approach.
- Continuous progress monitoring with tailored technology capability and self-evaluations across clinical and non-clinical hospital staff.
- Strong commitment from clinical and non-clinical hospital staff based on belief in the importance of technology to the industry.
- An aligned vision between management and hospital staff on the goal of the project.
Conclusion
Hospitals, both private and public, will undergo increased pressure to modernize their health information systems in the near future. In order to successfully execute these upgrades, an integrated planning and design framework is required. This framework should ensure proper identification of future needs, as well as enable the technology organization to implement the changes.
Arthur D. Little, facilitating your innovative potential in the healthcare sector
Arthur D. Little is uniquely positioned to support the healthcare sector in:
- Developing and implementing innovation strategies
- Identifying and implementing health information systems
- Reorganizing the healthcare sector and healthcare companies
- Identifying growth plans for new companies or projects
- Identifying new healthcare business models
We have extensive project experience in linking strategy, innovation, and transformation in the healthcare sector. Our internal experts combine extensive healthcare experience with local insight and industry expertise.
Our extensive network of external experts ensures that each client will leverage the best-possible expertise, in line with the challenges and the context the company is facing.
DOWNLOAD THE FULL REPORT
16 min read • Healthcare & life sciences, Information management
Hospital Information Systems for the digitally-enabled era
A new wave of innovation within healthcare is driving the need for more advanced, robust and scalable hospital information systems

DATE

Executive Summary
Healthcare is undergoing a paradigm shift driven by several factors. New models of care are emerging, focus is shifting from illness to wellness, and costs continue to climb amid rising demand for personalized, long-term care and the need for patients to participate in care management. Increasing expenditure on global healthcare delivery is unsustainable, which is making innovation and transformation imperative for sustainability. In this Viewpoint, Arthur D. Little analyzes how healthcare providers are starting to reorient their investments in hospital information systems’ other core technologies, and how technology vendors are adapting their solutions and services to meet these needs.
1
A new paradigm in healthcare delivery
The healthcare industry is undergoing radical change and disruption globally. New and emerging technologies such as artificial intelligence, powered analytics and diagnosis support, edge and secure cloud computing infrastructure, the internet of everything, and blockchain information exchange and interaction enablers, as well as practical technologies such as 3D printing and robotic surgery, are all changing how, where, and when healthcare can be delivered.
These developments combine to enable a fundamental shift towards coherently integrated health systems, in which multiple stakeholders (providers, patients, insurers, researchers and regulators) interact in a continuum, with a combined focus on enhancing both the care delivery methods and the outcomes being achieved. These shifts in healthcare delivery are characterized by some key features:
Emergence of “population health management”: Patients are no longer just treated as individual cases. With digital information exchanges, health data is being aggregated at community, national and regional levels. All stakeholders in the health ecosystem are creating mechanisms to access and share essential health-related information from disparate sources, allowing detection of key medical trends with greater speed and accuracy.
Patient centricity: Delivery of care is being tailored towards specific needs, preferences and patient values through increased digitized engagement models. Providers are focused on building personalized treatments, which create positive impact on outcomes and the overall patient experience.
Preventive- and lifetime-care approach: Advancements in medical knowledge and abundance of information dissemination methods are increasing patient awareness and participation in the management of their own wellness. Providers and regulators alike are focused on increasing people’s knowledge of medical conditions, symptoms and care options to encourage them to take a more proactive approach towards health management. Moreover, medical scientific advancements are going to make curative treatments available to patients with severe conditions.
Decentralized care: Patients now have access to high-quality care well beyond the confines of traditional geographical boundaries. Increasing use of telemedicine is creating a decentralized model of operation among health facilities. Increased availability and adoption of technologies in home care are extending care interaction well beyond the confines of the traditional hospital. This is transforming the traditional hospitalbased care-delivery model into an integrated but dispersed model of care management.
Non-invasive treatments: Advancements in medical technologies are creating a new generation of minimally invasive treatment options, thereby reducing dependence on complex physical infrastructure needs and reducing the duration of care delivery. Such treatment options, coupled with those to deliver such care outside the confines of the traditional hospital setting, are fundamentally altering how patients will experience health services in the future hospitals utilizing hospital information systems traditionally included 14 core modules to run their operations.
2
Factors driving the paradigm shift
A number of factors have contributed to this rapid shift in the health management and care delivery paradigm – rising costs of service delivery, the need to improve access to care, greater patient involvement in health management, and underlying technological advancements to improve outcomes. Moreover, health-service providers are facing challenges with health information exchange. Sharing health information can help health providers reduce readmissions, avoid medication errors, and even decrease duplicate testing. However, there are continued concerns about how to efficiently and effectively access data/ information for health professionals to conduct their jobs efficiently and safely. This also holds for other stakeholders, such as pharmaceutical companies and research institutions. In addition, there are growing concerns regarding how to keep data secure, ensure interoperability of various systems, remain competitive (e.g., sharing data among competitor health-service providers), and successfully implement the transformation program for the paradigm shift towards a digitally enabled era.
These factors have been strengthening with a shift in global demographics and increased demand for health services. Dramatic changes in lifestyle and increased average life spans that exponentially raise the demand for health services are making the underlying imbalances escalate.
We use the Middle East as an illustration. Its health systems are undergoing a significant transformation in the GCC (the Gulf Countries Cooperation, comprising the United Arab Emirates, Saudi Arabia, Oman, Kuwait, Bahrain and Qatar), which has experienced a growth in population, a shift towards an older age-group distribution, and high occurrence of lifestyle-related diseases. Local population growth bolstered by a large inflow of expats is expected to drive the GCC population count to 59.2 million by 2020 at a CAGR of 2.4 percent. Improved life expectancy has also led to a shift in the age-group distribution in which, by 2020, 15.3 percent of the population will be above the age of 50. The occurrence of lifestyle-related diseases such as diabetes, asthma and obesity have further augmented the need for healthcare services and facilities. Moreover, the high hospital-bed density in the GCC requires rethinking the way healthcare is delivered.
These changes – in addition to economic downturns and tight governmental budgets – have forced many health organizations (particularly hospitals) to change the way they deliver healthcare, as well as their operating and business models, and made it imperative to shift to a digitized healthcare system. In the midst of this digital transformation wave, the last decade has seen hospitals shifting their care-delivery models. Furthermore, with increasing maturity in technology adoption, most executives involved in the healthcare sector are increasingly focused on developing a new generation of smarter, digitally enabled hospitals, fundamentally rethinking hospital capabilities, and adopting an integrated approach to design, management and operations of their care delivery infrastructure.
3
The role of hospital information systems in the healthcare paradigm shift and challenges to driving digitization

Hospitals utilizing hospital information systems traditionally included 14 core modules to run their operations.
Hospital information systems play a vital role in digitization of care providers. Their benefits include, but are not limited to 1) improved information access, 2) increased healthcare professional productivity, 3) more efficient and accurate coding and billing, 4) higher-quality healthcare, 5) better clinical management (diagnosis and treatment), 6) reduced expenses associated with paper medical records, 7) fewer medical errors, 8) greater patient safety, 9) improved patient outcomes and 10) increased patient satisfaction.
Despite the prevalent benefits of digitization in the healthcare sector, many hospitals face difficulties in implementing new technologies in their existing service landscapes. Compared to other sectors, healthcare has traditionally been slower in adopting digitization. Three key challenges underpin the slow move towards adoption of digitalized solutions:
Technology: Integration of multiple IT systems, finding qualified and cost-effective service providers, and legacy issues.
Operations: Cultural change, particularly with senior doctors, staff, and the IT department.
Costs: Digitization is of investment intensive and added to the already-increasing cost service delivery.
Hence, the conceptualization and implementation of a digitalized hospital traditionally has been more complex than it appears on the surface. The first step towards implementing digitization in health organizations is to modernize and digitize their information systems for collecting, sharing, and analyzing large volumes of complex (and confidential) patient and other clinical information. Our vast amount of work in the Middle East and abroad supporting health organizations in innovating visions and strategies for digitalized hospitals has shown that most of these institutions find it difficult to understand and implement hospital information systems. However, this is more accurate in the Middle East than in Europe and the US. Many institutions in the Middle East lag behind in implementing these core technology capabilities. For example, adoption of electronic medical records (EMRs) in the Middle East is still trailing behind that of the US and Western Europe. This is mostly due to regulatory factors still taking shape, pushing providers towards increased EMR adoption and utilization. In the US, the 2009 HITECH Act was designed to bring hospitals into the modern era of technology and give them and physicians a reason to start using electronic records instead of paper. An incentive and penalty system was created as well.
To facilitate the adoption of these technologies, most GCC governments have laid out long-term strategic plans to upgrade their information systems. In KSA, for example, the “Comprehensive Health Program & National e-Health Strategy” has outlined 70+ projects focused on increasing HIS adoption among hospitals and PHCs, enhancing data centers and telecommunications equipment and enforcing stricter e-health standards and policies. However, hospitals still face many challenges in understanding, implementing and modernizing their hospital information systems. As most health systems shift towards adoption of these technologies, there needs to be cognizance of the rapid shift of these fundamental technologies. We have identified eight key trends that will fundamentally alter the health information system landscape. Senior executives and decision makers who are driving investments in hospital information systems need to make sure their ongoing investments cater to these emerging demands to future-proof these investments, since the pace of these advancements are significantly higher than the speed of implementation in most healthcare institutions.
4
Eight trends changing the HIS solution space
Upcoming trends in digital-health technologies, when integrated with hospital information systems, extend the boundaries of healthcare well outside the hospital walls, as well as deliver qualitative, quantitative and financial benefits to both patients and healthcare providers. Eight key trends in the digitization of healthcare are radically changing the HIS solution space:
Patient engagement: Hospital information systems are utilizing digital tools to increase participation and promote positive patient behavior. Through the use of mobile applications, interactive patient portals, text messages and e-mails, patient health outcomes are enhanced. These channels supply patients with important information, such as their personal health records and specific education about their medical conditions. They also allow patients to track their care plans, book appointments, manage prescriptions, and become more involved in treatment decision making. Allscripts, for example, has launched the FollowMyHealth® portal, which provides user-friendly navigation to encourage patients to stay connected. The engagement tool is also EHR-agnostic, which gives patients a single point of access, regardless of the different EHRs utilized by various providers.

Health analytics/artificial intelligence: Unprecedented growth of medical data generated from HIS has launched the era of health analytics and artificial intelligence in the healthcare domain. Information gathered and analyzed from patient records, drug administrations, operational data, insurance billing and regulatory sources can produce benefits in several areas:
- Performance management: Understanding of hospital performance along key metrics (related to outcomes and financials) to understand their clinical, operational and financial performance by department/clinical condition/ physician so they can identify and drive performance improvement initiatives.
- Pathway management: To optimize patient pathways within the network, as well as clinical pathways within the hospital, by coordinating care across settings.
- Clinical decision support: Utilization of patients’ clinical, physiological and longitudinal data to determine optimal diagnostic and treatment decisions so they can support clinical staff and decision boards.
- Precision medicine: Utilization of research and centralized data to promote enhanced diagnosing and personalized patient care.
- Safety practices: Use of predictive analytics to promote quality care and patient safety, e.g., early warning of a sepsis infection.
- Population health management: Utilization of analytics for use in epidemiology, e.g., linking EMRs with geographic information systems to identify healthcare trends in specific areas.
- Balancing length of stay and readmissions: Analysis of EMR data reveals trends that highlight patients likely to need additional treatment to prevent readmission, as well as patients who could be discharged earlier, so length of stay can be improved.
- Data security: Securing medical records by identifying changes in network traffic or behavior that could indicate a cyberattack.
- Insurance claims: Improving the efficiency of medical insurance claims by revealing claim trends and streamlining claims processing.
- Personalized medicine: Predictive modeling with EHR data is anticipated to drive personalized medicine and improve healthcare quality with its ability to leverage huge population sample data to identify patterns and trends and apply them to individual patient cases.
Wellness: Self-care through smartphones, tablet PCs and other communication devices has been experiencing unprecedented growth as ICT penetration and general medical awareness of patients have been increasing. Wellness supports patients in self-care through user-friendly digital applications that range from diet and weight loss to asthma care management. Lantern is a mobile application that provides support for emotional wellness through daily exercises and emotional coaching. It supports emotional wellness through cognitive behavioral therapy (CBT), helping users manage their problems by changing the way they think and behave, and also connects users with professionals through messaging and calling functionality. These digital applications can be integrated into HISs and support patient recovery by providing interactive treatment plans and monitoring progress.
Biosensing wearables: Biosensing wearables allow users to continuously measure a wide variety of metrics, and recent technological breakthroughs have made them affordable and accessible to the masses. These wearables come in an assortment of designs, from wristwatches and clothing to ingestibles and smart implants. These biosensors measure and track a diverse set of metrics: movement, heart rate, sleep, temperature, glucose, etc., and provide invaluable data points to users and healthcare providers that would have previously required intrusive methods to obtain. However, the sheer volume of available sensors and applications has presented healthcare providers with the challenge of software integration. Therefore, Leading HIS vendors have tackled this issue by partnering with technology platforms such as Validic. Validic is a cloud-based digital-health platform that connects providers, pharmaceutical companies, payers, wellness companies and health systems to over 400 in-home devices, wearables and patient-healthcare applications.
Telemedicine: Hospitals are moving towards utilization of telemedicine as part of the evolution into the patient-centric model. Previously, hospitals followed a centralized approach, which led to dramatic increases in operating costs and a great deal of travel inconvenience to patients living far from major hospitals. Through the use of telemedicine, patients and healthcare providers can now interact in real time through various communication channels and transmittal and storage of medical data, as well as remote monitoring. Epic, one of the largest US-based HIS providers, has partnered with Vidyo to provide remote healthcare services through computers and smart devices. Their product allows real-time video communication between clinicians and their patients or peers, within the same workflow tools they use for charting, accessing patient records and managing care. Telemedicine allows hospitals to decrease costs by reducing extra staff and space requirements, and increasing their ability to deliver care to larger volumes of customers.
Health information exchange: Healthcare information exchange (HIE) mobilizes healthcare data across organizations within a region, community or hospital system. There are three main types of HIE:
- Directed exchange: Sending and receiving secure information electronically between care providers to support coordinated care.
- Query-based exchange: Providers finding and/or requesting information on a patient from other providers – this is often used for unplanned emergency care.
- Consumer-mediated exchange: Patients aggregating and controlling the use of their health information among providers.
InterSystems has launched HealthShare as its strategic informatics platform for HIE. It allows effective and meaningful health-information sharing, whether for payers, within a hospital or hospital network, or across an entire region. The benefits include clear and secure access to records and improved visibility of overall population health, as well as reduced costs due to automated business processing, supported coordinatedcare management and, ultimately, reduced readmissions
However, there are continued concerns regarding how data/ information will be exchanged efficiently and effectively for health professionals to conduct their jobs proficiently and safely. This also holds for other stakeholders such as pharmaceutical companies and research institutions. There are other concerns around keeping the data secure, ensuring interoperability of various systems, competition (e.g., sharing data among competing health service providers), and implementing transformation programs for the paradigm shift towards a digitally enabled era.
Homecare: Advancements in technology have allowed patients to receive the care they need at home, avoiding unnecessary hospital visits. Patients are monitored in their homes with biosensors and PDAs, and connected 24/7 through software to emergency services, hospitals, clinics and hospice agencies. In addition, prescription management, full medical-record accessibility and digital support for homecare staff are used along the patient healing journey. Cerner’s HomeWorks® and RoadNotes® software solutions help hospice agencies and clinical staff deliver personalized homecare. Digital features support full life-cycle management of patient care, ease of transition between different levels of care, and compliance with regulatory requirements.
Cloud computing: Cloud computing can encourage digital healthcare adoption by reducing hospital information system startup and operational expenses. However, this comes at a cost of reduced flexibility. Practo’s Insta hospital information system is a software-as-a-service (SaaS) offering aimed at midmarket health providers. Its browser-based tools avoid lengthy and costly implementation time, and its modular product range caters to a wide variety of health providers.
There are several challenges and benefits related to cloud computing. Cloud computing does not necessarily promise lowering costs; it is more about accessibility and functionality. The main benefit of cloud computing is getting access to computing power and infrastructure that would be difficult and expensive to establish by own means, as it is not readily available in the market. The biggest challenge related to cloud computing is ensuring information security, especially when it comes to the CLOUD Act. This allows federal law enforcement to compel US-based technology companies, via warrant or subpoena, to provide requested data stored on servers, regardless of whether the data is stored inside or outside the US.
5
ADL’s view on HIS modernization
Hospitals aiming to digitize and evolve along the HC paradigm shift should aim to build hospital information systems beyond the core modules by moving towards adding more specialized modules (laundry, kitchen, anesthesia, and more), as well as connecting their existing HISs to external systems (HIE, telemedicine, biosensing wearables, etc.), depending on their needs. These updates pose challenges to healthcare providers in selecting products and vendors and implementing changes.
The first challenge that a hospital needs to address is identifying its current and future needs. Technology is ever-evolving, and a proper study of requirements is necessary to ensure selection of the right products.
The hospital should then assess which service and outsourcing models are most suitable to its operations in terms of cost and flexibility (on-premises, IAAS, PAAS, SAAS). Health providers must also look into vendor selection, adhering to single vendor options for all their systems versus going for a best-of-breed approach.
Advanced HIS platforms are heading in the direction of becoming more open in their architecture, allowing for direct integration with third-party tools and systems (for example, home-care solutions) and providing these to their patients through their websites, applications, etc. This concept will also align with the emerging patient-journey model. Hospitals could also evaluate partnering with providers such as online pharmacies, online consultation tools, and wellness management platforms, which would have a significant impact on the way they enable their service-delivery models to both patients and insurers.
Next, hospitals must address challenges that accompany implementation across the technology organization. These include: adapting system organization and workflow to suit the existing operating models or vice versa, reducing system downtime to a minimum, training staff and mitigating resistance to change, as well as ensuring data security. Addressing the challenges will require an integrated planning and design framework that includes not only technology, but also strategy, operations and infrastructure planning.
Finally, implementing HIS is not an IT project; rather, it is a large organizational transformation project requiring involvement of various stakeholders. Moreover, it is critical to involve the various stakeholders (such as health service providers) already at the outset of the HIS implementation (i.e., during the strategy development or supplier selection phase) to ensure a smooth, effective and successful HIS implementation.
Based on our experience working with hospital systems, we believe the key success factors required to achieve an effective upgrade are:
- Strong support from management and the drive to transform.
- Close alignment of the ICT system strategy with the overall objectives and vision of the hospital.
- Strong integration into clinical operations to drive new ways of working.
- Working towards a master plan with phased development rather than a scattered, piecemeal approach.
- Continuous progress monitoring with tailored technology capability and self-evaluations across clinical and non-clinical hospital staff.
- Strong commitment from clinical and non-clinical hospital staff based on belief in the importance of technology to the industry.
- An aligned vision between management and hospital staff on the goal of the project.
Conclusion
Hospitals, both private and public, will undergo increased pressure to modernize their health information systems in the near future. In order to successfully execute these upgrades, an integrated planning and design framework is required. This framework should ensure proper identification of future needs, as well as enable the technology organization to implement the changes.
Arthur D. Little, facilitating your innovative potential in the healthcare sector
Arthur D. Little is uniquely positioned to support the healthcare sector in:
- Developing and implementing innovation strategies
- Identifying and implementing health information systems
- Reorganizing the healthcare sector and healthcare companies
- Identifying growth plans for new companies or projects
- Identifying new healthcare business models
We have extensive project experience in linking strategy, innovation, and transformation in the healthcare sector. Our internal experts combine extensive healthcare experience with local insight and industry expertise.
Our extensive network of external experts ensures that each client will leverage the best-possible expertise, in line with the challenges and the context the company is facing.
DOWNLOAD THE FULL REPORT
